VA Rating for Sciatica: Understanding How the VA Evaluates Nerve Pain and Functional Limitations
Sciatica remains one of the most misunderstood conditions in the VA disability system, yet it affects thousands of veterans whose daily lives are shaped by nerve pain, mobility challenges, and functional limitations. The VA rating for sciatica is determined not by how severe the pain feels, but by how clearly medical documentation demonstrates nerve impairment and its impact on functional capacity.
Understanding how to challenge a low VA rating can help veterans who believe their sciatica disability rating doesn’t accurately reflect their functional limitations.
Table of Contents
- Understanding VA Sciatica Disability Ratings
- Medical Documentation and DBQ Process
- Secondary Conditions and Combined Ratings
- Strategic Steps for Rating Optimization
- Rating Chart and Evaluation Criteria
- Final Thoughts
TL;DR
- VA sciatica ratings typically range from 10-40%, with most veterans receiving 20-30% based on documented functional limitations
- Two primary diagnostic codes (8520 for nerve paralysis, 8620 for neuritis/neuralgia) significantly impact rating potential
- Comprehensive medical documentation through DBQs and objective testing forms the foundation of successful claims
- Secondary conditions from sciatica can substantially increase combined disability ratings
- Strategic documentation of daily functional limitations strengthens cases more than pain reports alone
- Independent medical evaluations provide objective evidence that aligns with VA rating criteria

Understanding VA Sciatica Disability Ratings
The VA evaluates sciatica as a neurological condition using specific diagnostic codes and percentage-based ratings from 0% to 100%. Most veterans receive ratings between 10-40% depending on documented functional impairment, with the system focusing on measurable limitations rather than subjective pain reports.
Sciatica affects millions of veterans, yet many don’t fully understand how the VA evaluates this debilitating condition. The VA treats sciatica as a neurological condition affecting the sciatic nerve, which means they’re looking for specific types of evidence. Ratings depend on how well documentation connects nerve damage to daily functional limitations.
Understanding the broader context of VA disability evaluations can help veterans navigate their sciatica claims more effectively, particularly when considering how VA disability ratings are determined across all conditions.
The Foundation of VA Sciatica Ratings
VA sciatica ratings follow a structured percentage system where most awards fall between 10-40%, with the average around 20%. While 100% ratings are rare for sciatica alone, they’re possible when combined with secondary conditions or when the condition causes complete functional disability. The rating received directly correlates to documented level of impairment and functional limitations.
Most veterans receive ratings between 10-30% for sciatica. The percentage reflects the severity of documented functional limitations, not the intensity of pain experience.
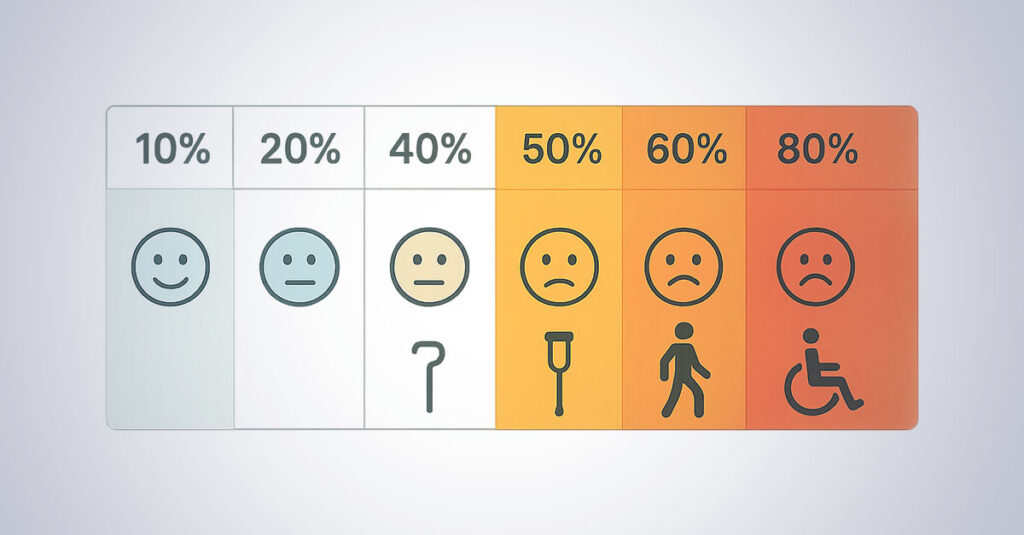
The rating scale typically looks like this:
- 10% Rating: Mild symptoms with occasional flare-ups that don’t significantly interfere with daily activities
- 20% Rating: Moderate symptoms affecting work capacity and daily functions
- 30% Rating: Significant functional limitations requiring lifestyle modifications
- 40% Rating: Severe impairment requiring assistive devices or mobility aids
The average VA rating for sciatica typically falls around 20%, but individual cases vary dramatically based on medical evidence quality and functional documentation. Veterans with similar symptoms can receive vastly different ratings based on documentation quality.
While 100% ratings for sciatica alone are uncommon, they’re possible. This typically happens when sciatica combines with secondary conditions or causes complete functional disability requiring constant care.
Diagnostic Codes That Determine Rating Potential
The VA uses two primary diagnostic codes for sciatica evaluation: Code 8520 for sciatic nerve paralysis (typically rated 60-80% for severe motor function loss) and Code 8620 for neuritis/neuralgia (usually rated 10-40% for pain-based symptoms). The chosen diagnostic code significantly impacts rating potential, making proper classification important for appropriate benefits.
The diagnostic code assigned to cases can significantly impact rating potential. The VA uses two primary codes, and understanding the difference is important.
Diagnostic Code 8520 (Sciatic Nerve Paralysis) covers complete sciatic nerve paralysis with severe motor function loss. This code typically yields higher ratings (60-80%) because it addresses significant functional impairments like foot drop and muscle weakness that are objectively measurable.
Diagnostic Code 8620 (Neuritis/Neuralgia) addresses sciatic neuritis and neuralgia, focusing on pain-based symptoms and sensory disturbances. These cases usually receive lower ratings (10-40%) unless accompanied by significant functional limitations.
The code selection process is based on specific symptoms and medical findings. However, many veterans don’t realize their conditions might qualify under the higher-rated code if properly documented.
Examiners determine which code applies based on medical evidence, but thorough documentation capturing all aspects of conditions, especially motor function impairments, can influence this determination.
| Diagnostic Code | Condition Type | Typical Rating Range | Key Symptoms |
| 8520 | Sciatic Nerve Paralysis | 60-80% | Motor function loss, foot drop, muscle weakness |
| 8620 | Neuritis/Neuralgia | 10-40% | Pain, numbness, tingling, sensory disturbances |
Medical Documentation and DBQ Process
Proper medical documentation through Disability Benefits Questionnaires (DBQs) forms the foundation of successful sciatica ratings. DBQs must capture specific functional limitations, objective findings, and pain levels while balancing subjective reports with measurable medical evidence like nerve conduction studies and imaging results. Strong documentation requires consistent treatment records, diagnostic testing, and clear connections between symptoms and functional impairment.
Medical documentation makes or breaks sciatica claims. The VA doesn’t just take statements at face value—they need comprehensive evidence that clearly establishes the condition’s impact on daily functioning.
The Disability Benefits Questionnaire (DBQ) serves as the primary tool for capturing this evidence. Think of it as the condition’s report card, where every section contributes to the final rating.
Veterans often benefit from understanding the comprehensive DBQ process before beginning their sciatica documentation journey.
Mastering the Sciatica DBQ Requirements
The sciatica DBQ captures essential elements including range of motion measurements, strength testing, sensory examination findings, and functional capacity assessments. Critical components must balance subjective pain reports with objective medical findings, requiring documentation of assistive device requirements and clear functional limitations that correlate directly to VA rating criteria.
The sciatica DBQ isn’t just a form—it’s a comprehensive evaluation tool that translates conditions into language the VA understands. Every section matters, and incomplete or poorly documented DBQs often result in lower ratings.
Essential DBQ components include:
- Range of motion measurements with specific degree limitations
- Strength testing results showing muscle weakness patterns
- Sensory examination findings documenting numbness or tingling areas
- Functional capacity assessments detailing daily activity limitations
- Documentation of assistive device requirements and usage frequency
Balancing subjective pain reports with objective medical findings is important. While pain experience is valid and important, the VA needs measurable evidence to assign ratings. Nerve conduction studies showing slowed transmission, imaging results revealing nerve compression, and EMG findings indicating muscle denervation carry significant weight.
Examining physicians should document not just what is reported, but what they observe during examinations. Antalgic gait patterns, protective posturing, and visible functional limitations during testing strengthen cases considerably.
A veteran with sciatica receives a 20% rating when their DBQ documents “occasional pain and mild functional limitations.” However, a similar veteran receives a 40% rating because their DBQ specifically states “constant severe pain radiating down left leg, requiring use of cane for distances over 100 yards, documented muscle weakness in left foot dorsiflexion testing at 3/5 strength, and EMG showing denervation in L5 distribution.” The difference in documentation detail directly influenced the rating outcome.
Building Strong Medical Evidence
Strong medical evidence requires comprehensive treatment records, diagnostic testing results, and clear connections between symptoms and functional impairment. MRI scans showing nerve compression, nerve conduction studies, and EMG results significantly strengthen claims, while treatment history documentation including physical therapy, medications, and procedures demonstrates condition severity and persistence.
Medical evidence quality often determines rating success more than symptom severity. Veterans with debilitating symptoms can receive low ratings due to poor documentation, while others with moderate symptoms receive higher ratings because of comprehensive medical records.
Imaging and Testing Requirements form the objective foundation of claims. MRI scans showing clear nerve compression provide visual evidence of the condition’s physical basis. Nerve conduction studies demonstrating slowed transmission speeds offer measurable proof of nerve damage. EMG results indicating muscle denervation show the functional impact of conditions.
Treatment History Documentation tells the story of condition persistence and severity. Physical therapy notes detailing limitations and progress (or lack thereof) demonstrate ongoing functional impact. Medication trials show the level of intervention required to manage symptoms. Injection procedures and surgical interventions indicate conservative treatment failures and condition severity.
Documentation must clearly establish causation—how sciatica directly affects specific daily activities, work capacity, sleep patterns, and overall quality of life. Vague statements like “causes pain” don’t help. Specific examples like “unable to stand for more than 15 minutes without severe pain radiating down left leg” provide actionable evidence.
Treatment records should show consistency over time. Sporadic complaints followed by long gaps in treatment can undermine claim credibility. Regular, consistent documentation of symptoms and limitations strengthens cases significantly.
Veterans should understand that comprehensive medical evidence serves as the cornerstone of successful disability claims across all conditions, including sciatica.
Medical Evidence Checklist:
- ☐ MRI or CT scans showing nerve compression
- ☐ Nerve conduction study results
- ☐ EMG findings documenting muscle denervation
- ☐ Complete physical therapy records with functional assessments
- ☐ Medication trial documentation and effectiveness notes
- ☐ Injection procedure records (epidural, trigger point, etc.)
- ☐ Surgical consultation notes or operative reports
- ☐ Consistent treatment records spanning multiple months/years
- ☐ Specific functional limitation documentation
- ☐ Sleep study results if sleep disruption is documented
Secondary Conditions and Combined Ratings
Sciatica frequently leads to secondary conditions that can increase overall disability ratings through the VA’s combined rating system. Common secondary conditions include musculoskeletal problems from altered gait patterns and mental health conditions from chronic pain. The VA uses a specific mathematical formula for combining ratings that doesn’t simply add percentages but uses a diminishing returns approach, making strategic secondary condition documentation important for comprehensive benefits.
Sciatica rarely exists in isolation. The condition often triggers a cascade of secondary problems that can significantly impact overall disability ratings when properly documented and connected.
Understanding the combined rating system is important because it can transform a modest 20% sciatica rating into a much higher combined percentage when secondary conditions are included.
Identifying Common Secondary Conditions
Secondary conditions from sciatica include musculoskeletal problems like hip, knee, and ankle issues from altered gait patterns, plus lower back conditions from compensatory movements. Mental health secondary conditions such as depression, anxiety, and sleep disorders can develop from chronic pain and qualify for separate disability ratings when properly documented and connected to the primary sciatica condition.
Secondary conditions develop naturally from sciatica’s functional limitations and the body’s compensatory responses. Recognizing these patterns helps in documenting additional ratable conditions.
Musculoskeletal Secondary Conditions are extremely common. When sciatica affects gait, weight and movement patterns unconsciously shift to avoid pain. This compensation leads to hip problems from altered weight distribution, knee issues from changed walking mechanics, and ankle problems from modified foot placement patterns.
Lower back conditions often worsen due to compensatory movements and muscle imbalances. The body tries to protect the affected sciatic nerve by changing how it moves, which places additional stress on other spinal structures.
Mental Health Secondary Conditions develop from the psychological impact of chronic pain. Depression and anxiety are common responses to persistent pain and functional limitations. Sleep disorders frequently result from pain-related sleep disruption, creating a cycle that affects overall mental health.
These aren’t separate, unrelated conditions—they’re direct consequences of sciatica. The key is establishing clear medical connections between primary conditions and these secondary effects.
Documentation should show the timeline of symptom development, with secondary conditions appearing after sciatica diagnoses. Treatment records should reflect the interconnected nature of these conditions and how they compound overall functional limitations.
Veterans dealing with pain-related mental health challenges may benefit from understanding how the VA evaluates depression as a secondary condition to chronic pain conditions like sciatica.
A Marine veteran initially received a 30% rating for service-connected sciatica. Through proper documentation, he successfully added secondary conditions: 20% for depression related to chronic pain, 10% for sleep apnea worsened by pain-related sleep positioning, and 10% for right knee strain from altered gait. His combined rating increased from 30% to 60%, significantly increasing his monthly compensation.
Understanding Combined Rating Mathematics
The VA uses a specific combined rating formula that doesn’t simply add percentages together but employs a diminishing returns approach. For example, a 30% sciatica rating combined with a 20% secondary condition results in a 44% combined rating (rounded to 40%), not 50%. Understanding this calculation helps veterans strategically pursue secondary conditions that meaningfully impact their combined rating.
The VA’s combined rating system often confuses veterans because it doesn’t work like simple addition. Understanding this calculation helps in making strategic decisions about pursuing secondary conditions.
The system uses a diminishing returns approach where each additional rating has less impact than the previous one. A 30% sciatica rating combined with a 20% secondary condition doesn’t equal 50%—it results in a 44% combined rating, which rounds to 40%.
Here’s how it works: The VA considers the most severe condition first, then applies subsequent ratings to the remaining “efficiency” percentage. With a 30% primary rating, there’s 70% remaining efficiency. The 20% secondary condition applies to that 70%, adding 14% (20% of 70%) for a total of 44%.
This system means pursuing multiple smaller secondary conditions can be more beneficial than hoping for one large rating increase. Three 10% secondary conditions combined with a 20% primary rating can yield a significantly higher combined percentage than a single 30% rating.
The rounding rules also matter. Combined ratings ending in 1-4 round down, while those ending in 5-9 round up. A 44% combined rating rounds to 40%, but a 45% would round to 50%—a significant difference in compensation.
Strategic secondary condition documentation becomes important when close to rating thresholds. That additional 10% secondary condition might push from 40% to 50%, substantially increasing monthly compensation.
| Primary Rating | Secondary Rating | Mathematical Calculation | Combined Rating | Final Rounded Rating |
| 30% | 20% | 30 + (70 × 0.20) = 44% | 44% | 40% |
| 20% | 10% + 10% | 20 + (80 × 0.10) + (72 × 0.10) = 35.2% | 35% | 30% |
| 40% | 30% | 40 + (60 × 0.30) = 58% | 58% | 60% |
| 30% | 10% + 10% + 10% | 30 + 7 + 6.3 + 5.67 = 49% | 49% | 50% |
Strategic Steps for Rating Optimization
Veterans can optimize their sciatica ratings through systematic documentation strategies including comprehensive medical records gathering, detailed functional limitation documentation, and independent medical evaluations. The process involves collecting all treatment records without gaps, maintaining detailed records of daily limitations with specific examples, and obtaining thorough objective medical examinations that align with VA rating criteria.
Optimizing sciatica ratings isn’t about gaming the system—it’s about ensuring conditions are properly documented and evaluated according to their true impact on life.
The difference between a successful claim and a disappointing rating often comes down to preparation and documentation strategy. Veterans who approach this systematically typically achieve better outcomes than those who simply hope for the best.
Veterans seeking to improve their ratings should understand the common pitfalls by reviewing typical VA disability filing mistakes that can undermine even strong medical cases.
Your Documentation Strategy Roadmap
Effective documentation strategy involves three critical steps: comprehensive medical records gathering to ensure no gaps in the medical timeline, functional limitation documentation with specific daily activity impacts, and independent medical evaluations from qualified physicians who can provide thorough DBQ completion and detailed functional assessments aligned with VA rating criteria.
Step 1: Comprehensive Medical Records Gathering forms claim foundations. Collecting every piece of medical documentation related to sciatica is necessary, including initial injury reports, emergency room visits, specialist consultations, imaging studies, and ongoing treatment records.
Seemingly minor documentation shouldn’t be overlooked. Physical therapy notes often contain detailed functional assessments that support higher ratings. Medication records show treatment intensity and symptom persistence. Even brief mentions of sciatica symptoms in unrelated medical visits can establish timeline continuity.
Gaps in medical timelines can weaken claims significantly. When periods exist without treatment, being prepared to explain why (financial constraints, military deployment, lack of available care, etc.) is important. Consistent documentation over time demonstrates condition persistence and severity.
Step 2: Functional Limitation Documentation translates medical conditions into real-world impact. The VA needs specific examples of how sciatica affects daily life, not general statements about pain or discomfort.
Maintaining detailed records of daily limitations with specific examples helps:
- “Cannot stand for more than 10 minutes without severe pain shooting down right leg”
- “Unable to lift objects over 15 pounds due to increased sciatic pain”
- “Requires frequent position changes during 8-hour workday”
- “Sleep disrupted 3-4 times nightly due to leg pain and numbness”
Documenting how conditions affect work performance, household activities, recreational pursuits, and social interactions matters. The more specific and measurable the limitations, the stronger the documentation becomes.
Step 3: Independent Medical Evaluation provides objective, comprehensive assessment from qualified physicians experienced in VA disability evaluations. These evaluations can fill documentation gaps and provide thorough DBQ completion that aligns with VA rating criteria.
Independent evaluations offer several advantages: comprehensive examination focused specifically on disability claims, detailed functional assessments that correlate to rating criteria, objective documentation from neutral medical professionals, and thorough DBQ completion by physicians familiar with VA requirements.
Choosing qualified physicians who understand VA disability evaluation standards and can provide detailed, objective assessments that accurately reflect functional limitations is important.
Strategic Documentation Timeline:
- ☐ Month 1: Gather all existing medical records
- ☐ Month 2: Begin detailed daily symptom logging
- ☐ Month 3: Schedule comprehensive independent medical evaluation
- ☐ Month 4: Obtain any missing diagnostic tests (MRI, EMG, etc.)
- ☐ Month 5: Document secondary condition connections
- ☐ Month 6: Compile complete claim package with all evidence
An Army veteran initially received a 10% rating for sciatica with minimal documentation. After implementing a strategic documentation approach over six months—gathering complete medical records, maintaining a detailed symptom diary, and obtaining an independent medical evaluation—he successfully increased his rating to 40% on appeal, resulting in an additional $400+ monthly compensation.
Rating Chart and Evaluation Criteria
The VA sciatica rating chart provides specific percentage assignments based on measurable functional limitations, pain severity, and objective medical findings. The chart translates medical findings into standardized ratings from 10% (mild incomplete paralysis with occasional pain) to 40%+ (severe incomplete paralysis with constant pain requiring assistive devices). Pain assessment integrates frequency, intensity, and functional impact through objective indicators rather than subjective reports alone.
The VA sciatica rating chart isn’t just a reference tool—it’s a roadmap to understanding exactly what evidence is needed for specific rating levels. Each percentage corresponds to specific functional limitations and objective findings that examiners must document.
Understanding these criteria helps focus documentation efforts on the evidence that matters most for target rating levels.
Decoding the Sciatica Rating Chart
The rating chart breakdown shows 10% ratings for mild incomplete paralysis with minimal daily interference, 20-30% ratings for moderate incomplete paralysis affecting work capacity with measurable muscle weakness, and 40%+ ratings for severe incomplete paralysis with constant pain requiring medication management and assistive devices. Each level requires specific documentation of functional limitations and objective medical findings.
10% Rating Criteria represents the entry level for sciatica disability ratings. This applies to mild incomplete paralysis with occasional pain episodes that don’t significantly interfere with daily activities. Minimal sensory loss exists and no requirement for assistive devices during normal functioning.
The key word here is “occasional.” When symptoms are constant or frequently recurring, higher ratings likely apply. Documentation should show symptom frequency and intensity patterns over time.
20-30% Rating Criteria covers moderate incomplete paralysis with regular pain affecting work capacity. This level requires some muscle weakness measurable through testing and periodic need for mobility assistance during flare-ups.
The distinction between 20% and 30% often comes down to documentation quality and functional impact severity. Regular pain that affects work capacity suggests 20%, while significant functional limitations requiring lifestyle modifications lean toward 30%.
40% and Above Rating Criteria addresses severe incomplete paralysis with constant pain requiring regular medication management. This level involves significant muscle weakness affecting major life activities and consistent need for assistive devices or mobility aids.
The jump to 40% represents a significant threshold in VA ratings, both in terms of required evidence and compensation levels. Documentation must clearly establish constant symptoms, medication dependence, and consistent functional limitations requiring assistive devices.
The highest VA rating for sciatica can reach 60-80% under diagnostic code 8520 when evidence shows complete or near-complete sciatic nerve paralysis with severe motor function loss, foot drop, and significant muscle atrophy. What the VA disability rating for sciatica will be depends entirely on documented functional limitations and which diagnostic code applies to specific cases.
Higher ratings (60-80%) under diagnostic code 8520 require evidence of complete or near-complete sciatic nerve paralysis with severe motor function loss, foot drop, and significant muscle atrophy.
Pain Assessment Within the Rating Framework
Pain evaluation in VA sciatica ratings considers frequency, intensity, duration, and functional impact through objective indicators rather than subjective reports alone. Measurable pain indicators include antalgic gait patterns, protective posturing, medication requirements, sleep disruption documentation, and observable functional limitations during examination. Pain severity directly influences rating percentages when correlated with functional limitations and documented interference with daily activities.
Pain assessment goes beyond “it hurts” to measurable, observable indicators that examiners can document objectively. The VA needs evidence they can see, measure, and verify.
Objective Pain Indicators include antalgic gait patterns (limping or altered walking to avoid pain), protective posturing during movement, medication requirements and effectiveness, sleep disruption documentation, and observable functional limitations during examination.
Gait patterns tell a story. When weight unconsciously shifts, stride length shortens, or one leg is favored, these patterns provide objective evidence of pain’s functional impact. Examiners document these observations as measurable findings.
Protective posturing—how movement occurs to avoid pain—offers another objective indicator. Guarding movements, hesitation before position changes, and visible discomfort during specific activities provide evidence beyond subjective reports.
Pain Impact on Rating becomes significant when correlated with functional limitations, treatment requirements, and documented interference with occupational and daily living activities. Isolated pain reports without functional correlation rarely drive higher ratings.
The connection between pain and function is important. Pain that prevents standing for extended periods, limits lifting capacity, or requires frequent position changes has measurable functional impact. Pain that simply “bothers” without clear functional limitations carries less rating weight.
Medication requirements provide objective evidence of pain severity. The type, dosage, frequency, and effectiveness of pain medications help establish symptom intensity and persistence. Failed conservative treatments and progression to stronger medications demonstrate condition severity.
Sleep disruption from pain creates a documented pattern that examiners can verify through medical records and functional assessments. Frequent awakening, position changes during sleep, and daytime fatigue from poor sleep quality provide measurable evidence of pain’s life impact.
Recent clinical research published in the New England Journal of Medicine found that “pregabalin did not relieve sciatic pain or improve related clinical measures, as compared with placebo, over the course of 8 weeks”, demonstrating the complexity of sciatica treatment and supporting the need for comprehensive documentation when conservative treatments fail to provide relief.
How REE Medical Supports Your Sciatica Documentation Journey
When navigating the complex world of VA sciatica ratings, having access to thorough, objective medical evaluations can make the difference between an accurate rating and an undervalued claim.
REE Medical coordinates independent medical evaluations that focus specifically on documenting sciatica-related functional limitations according to VA criteria. Our network of experienced physicians understands exactly what evidence the VA needs to see and how to document it properly.
We don’t file claims or guarantee outcomes—that’s not our role. Instead, we coordinate comprehensive medical assessments that accurately capture the condition’s true impact on daily functioning. Our evaluations provide the detailed, objective documentation that strengthens cases within full legal and ethical boundaries.
Veterans can learn more about coordinating VA-compliant medical evaluations by contacting REE Medical for an informational consultation. REE Medical’s team explains the documentation coordination process and connects veterans with independent, licensed medical providers.
Veterans considering independent medical evaluations should understand how independent medical opinions can strengthen their disability claims through objective professional assessment.
Final Thoughts
Successfully navigating VA sciatica ratings requires understanding the systematic approach the VA uses to evaluate functional limitations rather than just pain levels. The key to appropriate ratings lies in comprehensive documentation that clearly connects medical conditions to specific daily functional impacts, strategic pursuit of secondary conditions, and obtaining thorough medical evaluations that align with VA criteria.
While the process can seem overwhelming, veterans who approach it systematically with proper medical documentation typically achieve ratings that accurately reflect their condition’s true impact on their lives.
Sciatica ratings should reflect the real impact this condition has on daily life. Too many veterans accept lower ratings simply because they don’t understand what evidence the VA needs or how to present it effectively.
The difference between a 10% rating and a 30% rating often comes down to documentation quality, not symptom severity. Veterans with similar conditions can receive vastly different ratings based on how well their functional limitations are documented and connected to their medical evidence.
Secondary conditions can significantly impact combined ratings. Hip problems from altered gait, sleep issues from chronic pain, or mental health impacts from dealing with persistent symptoms shouldn’t be overlooked. These aren’t separate issues—they’re direct consequences of sciatica that deserve recognition and compensation.
The VA disability system isn’t perfect, but it does follow consistent rules. When those rules are understood and preparation occurs accordingly, veterans are much more likely to receive ratings that accurately reflect their condition’s impact on their lives.

Disclosure
DISCLAIMER: REE Medical, LLC is not a Veterans Service Organization (VSO) or a law firm and is not affiliated with the U.S. Veterans Administration (“VA”). Results are not guaranteed, and REE Medical, LLC makes no promises. REE Medical’s staff does not provide medical advice or legal advice, and REE Medical is not a law firm. Any information discussed, such as, but not limited to, the likely chance of an increase or service connection, estimated benefit amounts, and potential new ratings, is solely based on past client generalizations and not specific to any one patient. The doctor has the right to reject and/or refuse to complete a Veteran’s Disability Benefit Questionnaire if they feel the Veteran is not being truthful. The Veteran’s Administration is the only agency that can make a determination regarding whether or not a Veteran will receive an increase in their service-connected disabilities or make a decision on whether or not a disability will be considered service-connected. This business is not sponsored by, or affiliated with, the United States Department of Veterans Affairs, any State Department of Military and Veterans Affairs, or any other federally chartered veterans service organization.