VA Rating for Radiculopathy: What Veterans Need to Know About Getting the Compensation You Deserve
Radiculopathy affects thousands of veterans nationwide, with VA ratings ranging from 0% to 90% depending on the severity, frequency, and duration of symptoms. Understanding how to navigate the complex VA rating system for nerve root conditions provides valuable insight into the disability compensation process and what medical evidence the VA reviews when making rating determinations.
Understanding VA disability compensation rates helps veterans calculate potential benefits from radiculopathy ratings and plan accordingly.
Table of Contents
- Understanding Radiculopathy and VA Disability Ratings
- Regional Radiculopathy: Cervical, Thoracic, and Lumbar Conditions
- Comorbid Conditions and Secondary Service Connection
- Navigating the VA Claims Process for Radiculopathy
- Specialized Rating Considerations and Advanced Topics
- How REE Medical Supports Veterans with Radiculopathy Claims
- Final Thoughts
TL;DR
- Radiculopathy affects nerve roots and can qualify for VA disability ratings ranging from 10% to 40% based on severity and functional limitations
- Service connection requires clear documentation linking military service to the nerve condition through direct injury, aggravation, or secondary development
- Different spinal regions (cervical, thoracic, lumbar) have specific evaluation criteria, with cervical and lumbar being most common among veterans
- Secondary conditions like depression, joint problems, and sleep disorders can develop from radiculopathy and warrant additional VA ratings
- Bilateral radiculopathy qualifies for bilateral factor calculations, potentially increasing overall disability percentage
- Strong claims require comprehensive medical documentation including imaging studies, nerve conduction tests, and detailed functional assessments
- Combined ratings with other spinal conditions require strategic approaches to maximize compensation while avoiding pyramiding
- Independent medical evaluations can provide the detailed documentation necessary for accurate VA rating decisions
Radiculopathy represents a significant neurological condition affecting thousands of veterans, characterized by nerve root dysfunction that creates pain, weakness, and numbness along specific nerve pathways. The VA’s approach to rating these conditions requires understanding both the medical complexity of nerve damage and the specific criteria used to evaluate disability compensation.
Defining Radiculopathy in the VA Context
The Department of Veterans Affairs recognizes radiculopathy as a distinct neurological condition requiring specific diagnostic criteria and comprehensive documentation for proper evaluation. Understanding how the VA classifies and approaches these nerve root conditions helps clarify the disability compensation process.
Medical Classification and Symptoms
Radiculopathy manifests through nerve root compression or irritation, creating characteristic symptoms that the VA evaluates using established diagnostic codes and severity criteria. These symptoms directly impact functional capacity and quality of life, forming the foundation for disability rating determinations.
Nerve root dysfunction doesn’t just cause discomfort—it fundamentally alters how the body functions. When nerve roots become compressed or irritated, radiating pain occurs along specific nerve pathways, often accompanied by muscle weakness and sensory changes.
The VA recognizes several key symptom patterns:
- Sharp, shooting pain that travels from the spine into extremities
- Muscle weakness affecting specific muscle groups
- Numbness or tingling in predictable nerve distributions
- Reduced reflexes in affected areas
- Functional limitations in daily activities
These symptoms aren’t random—they follow anatomical patterns that help medical professionals identify which nerve roots are affected. The VA uses this information to assign appropriate diagnostic codes and determine disability percentages.
Consider a veteran who developed C6 radiculopathy after a parachute landing injury. They experience weakness in their thumb and index finger, making it difficult to grip tools or write legibly. The VA examiner tests their grip strength at 15 pounds compared to the normal 60 pounds for their age group, documenting objective evidence of nerve dysfunction. The VA ultimately assigned a 30% disability rating based on this documented functional limitation.
Service Connection Requirements
Establishing service connection for radiculopathy demands clear documentation linking military service to the current nerve condition, whether through direct trauma, aggravation of pre-existing conditions, or secondary development from other service-connected disabilities.
Military service creates unique physical demands and injury risks that civilian populations rarely face. Heavy lifting, prolonged sitting in vehicles, parachute landings, and combat injuries all contribute to spinal stress that can damage nerve roots.
Direct service connection occurs when:
- A specific injury during service damaged nerve roots
- Medical records document the initial injury and subsequent nerve symptoms
- There’s a clear timeline from service injury to current radiculopathy
Secondary service connection applies when radiculopathy develops from another service-connected condition. For example, when veterans have service-connected back injuries that later cause nerve compression, the resulting radiculopathy can be rated separately.
Aggravation claims work when pre-existing nerve issues existed that military service made worse. The VA must determine what portion of current disability stems from service aggravation versus natural progression.
Veterans seeking to establish service connection for nerve conditions may benefit from understanding nexus letter requirements that properly document the relationship between military service and current radiculopathy symptoms.
Documentation Standards
Proper VA rating requires comprehensive medical documentation that clearly demonstrates the extent and impact of nerve root dysfunction through imaging studies, neurological examinations, and functional assessments.
Strong radiculopathy claims rest on solid medical evidence. Subjective symptom descriptions alone provide limited value—objective medical findings that support claims become necessary.
Essential documentation includes:
- MRI or CT scans showing nerve compression or spinal abnormalities
- Nerve conduction studies demonstrating electrical dysfunction
- EMG testing revealing muscle denervation patterns
- Detailed neurological examinations documenting reflexes, strength, and sensation
- Functional capacity evaluations measuring real-world limitations
Medical records should present a complete picture of how radiculopathy affects daily life. Generic statements about “back pain” won’t suffice—specific documentation of nerve-related symptoms and their functional impact is necessary.
Radiculopathy Documentation Checklist:
- ☐ Current MRI or CT imaging within 12 months
- ☐ Nerve conduction study results
- ☐ EMG testing documentation
- ☐ Detailed neurological examination findings
- ☐ Functional capacity evaluation
- ☐ Physician’s opinion on service connection
- ☐ Timeline of symptom progression
- ☐ Impact statements on daily activities
Understanding the importance of medical evidence becomes important when building comprehensive radiculopathy claims that accurately reflect functional limitations.
VA Rating Criteria and Diagnostic Codes
The VA employs specific diagnostic codes under the Schedule for Rating Disabilities to evaluate radiculopathy, with ratings determined by symptom severity, functional limitations, and anatomical location of nerve involvement.
| Symptom Severity | Typical VA Rating | Key Characteristics |
| Mild | 10-20% | Minor pain, tingling, minimal functional impact |
| Moderate | 20-40% | Significant numbness, moderate pain, notable limitations |
| Severe | 40-50% | Muscle atrophy, severe weakness, major functional loss |
| Complete Paralysis | 60-90% | Total loss of function, equivalent to amputation |
General Rating Principles
VA ratings for radiculopathy typically range from 10% to 40% based on the severity of symptoms and degree of functional impairment, with specific criteria for mild, moderate, and severe incomplete paralysis of affected nerve groups. These standardized rating levels provide consistency across different cases while accounting for individual symptom severity.
The VA doesn’t rate radiculopathy based on pain alone—ratings focus on measurable functional limitations. Ratings depend on how severely nerve dysfunction affects ability to use affected body parts.
Rating levels typically break down as:
- 10%: Mild incomplete paralysis with minimal functional impact
- 20%: Moderate incomplete paralysis affecting daily activities
- 40%: Severe incomplete paralysis with significant functional limitations
“Incomplete paralysis” doesn’t mean partial paralysis in the traditional sense. It refers to nerve dysfunction that reduces strength, sensation, or coordination without complete loss of function.
VA examiners test specific functions like grip strength, walking ability, and fine motor control. Ratings reflect how much nerve damage interferes with these measurable activities.
Bilateral Rating Considerations
When radiculopathy affects both sides of the body, the VA applies bilateral factor calculations that can significantly increase overall disability compensation by adding percentage points to the combined rating calculation.
Bilateral radiculopathy creates unique rating opportunities. When nerve dysfunction affects both sides of the body, the calculation goes beyond two separate ratings—a mathematical advantage applies.
The bilateral factor adds 10% of the combined value of bilateral disabilities to the overall rating. This calculation method can mean substantial additional compensation.
For example, if veterans have 20% ratings for radiculopathy in both legs, the combined bilateral rating becomes higher than the standard 36% from combining two 20% ratings. The bilateral factor increases it further.
This applies when:
- Bilateral lumbar radiculopathy affects both legs
- Bilateral cervical radiculopathy affects both arms
- Any symmetrical nerve condition affects paired extremities
Anatomical Classifications and Rating Groups
The VA categorizes radiculopathy based on anatomical location and affected nerve groups, with distinct rating criteria for upper, middle, and lower radicular groups that directly influence disability percentages. Each anatomical region presents unique functional challenges that the VA evaluates differently.
Upper Radicular Group Assessment
Upper radicular group involvement affects nerve roots C5-C8 and T1, impacting shoulder, arm, and hand function with VA ratings reflecting the degree of motor and sensory impairment in these critical areas for daily functioning and employment.
Upper extremities handle most daily tasks, making cervical radiculopathy particularly disabling. When nerve roots C5 through T1 become damaged, function in shoulders, arms, and hands is lost.
The VA pays special attention to:
- Grip strength measurements
- Fine motor control for writing and manipulation
- Shoulder range of motion and stability
- Ability to lift and carry objects
- Hand coordination for detailed tasks
Upper radicular group problems often affect ability to work, especially in jobs requiring manual dexterity or overhead reaching. The VA considers these employment impacts when determining ratings.
Cervical radiculopathy frequently causes symptoms that radiate into specific fingers, following predictable nerve patterns. C6 radiculopathy affects the thumb and index finger, while C8 involvement impacts the ring and little fingers.
Middle Radicular Group Evaluation
Middle radicular group conditions affect thoracic nerve roots and, while less commonly rated, can significantly impact trunk stability and respiratory function when present, requiring careful evaluation of core strength and breathing capacity.
Thoracic radiculopathy gets less attention than cervical or lumbar conditions, but it can be equally disabling. The thoracic spine supports the entire trunk and affects breathing mechanics.
Middle radicular group symptoms include:
- Chest wall pain that wraps around the torso
- Trunk instability affecting balance and posture
- Respiratory muscle weakness in severe cases
- Difficulty with twisting and bending motions
These conditions often get misdiagnosed as heart problems or lung issues because the pain can mimic cardiac or pulmonary symptoms. Proper diagnosis requires understanding thoracic nerve anatomy and distribution patterns.
Lower Radicular Group Impact
Lower radicular group involvement affects lumbar and sacral nerve roots (L1-S3), commonly resulting in lower back pain, leg weakness, and functional limitations that form the primary basis for VA disability ratings in the most prevalent form of veteran radiculopathy.
Lumbar radiculopathy represents the most common nerve condition among veterans, affecting ability to walk, stand, and perform basic daily activities. The sciatic nerve, formed from multiple lumbar nerve roots, becomes a frequent source of disability.
Lower radicular symptoms typically include:
- Sharp pain radiating from the back into the legs
- Weakness in specific leg muscles
- Numbness or tingling in predictable patterns
- Difficulty walking long distances
- Problems with balance and coordination
The VA evaluates how these symptoms affect mobility and independence. Walking distance, need for assistive devices, and how often symptoms force rest or activity modifications all factor into rating determinations.
L5 radiculopathy often causes foot drop, making it difficult to lift toes while walking. S1 involvement typically affects calf muscles and Achilles reflex. These specific patterns help establish the medical basis for ratings.

Regional Radiculopathy: Cervical, Thoracic, and Lumbar Conditions
Different spinal regions present unique challenges for VA rating, with cervical and lumbar radiculopathy being most prevalent among veterans due to the physical demands of military service. Each region requires specific evaluation criteria and documentation approaches, as the functional impacts vary significantly between neck, mid-back, and lower back nerve involvement.
Cervical Radiculopathy VA Rating
Cervical radiculopathy affects nerve roots in the neck region, often causing upper extremity symptoms that can significantly impact ability to work and perform daily activities, requiring careful evaluation of arm and hand function for appropriate disability rating.
Upper Extremity Impact Assessment
VA ratings for cervical radiculopathy focus on functional limitations in the arms, hands, and shoulders, with specific attention to grip strength, range of motion, and ability to perform fine motor tasks that are essential for employment and daily living activities.
Cervical nerve damage creates a cascade of problems throughout upper extremities. Unlike other spinal conditions that might cause localized pain, cervical radiculopathy directly affects ability to use arms and hands effectively.
VA examiners test several key functions:
- Grip strength using a dynamometer
- Pinch strength for fine motor tasks
- Range of motion in shoulders, elbows, and wrists
- Coordination tests like finger-to-nose movements
- Ability to manipulate small objects
These tests aren’t just medical formalities—they measure capacity for employment and daily activities. Reduced grip strength affects everything from opening jars to using tools. Poor coordination makes writing, typing, and detailed work nearly impossible.
Cervical radiculopathy often affects dominant hand function more severely, creating additional disability considerations. When conditions affect dominant sides, functional limitations become more pronounced than when the same condition affects non-dominant sides.
A Marine Corps veteran developed cervical radiculopathy after a vehicle rollover in Afghanistan. His C7 nerve root compression resulted in weakness affecting his middle finger and triceps muscle. During his C&P exam, his grip strength measured 25 pounds on the affected side versus 55 pounds on the unaffected side. He reported difficulty using power tools in his construction job and trouble lifting objects overhead. The VA ultimately assigned a 30% disability rating based on this documented functional impairment.
Secondary Condition Development
Cervical radiculopathy often leads to secondary conditions such as headaches, sleep disorders, and psychological impacts that may warrant additional VA ratings and compensation beyond the primary nerve condition rating.
Common secondary conditions include:
- Cervicogenic headaches from nerve irritation
- Sleep disorders due to positional pain
- Depression and anxiety from chronic pain
- Shoulder impingement from altered movement patterns
- Carpal tunnel syndrome from compensatory hand positioning
Each secondary condition requires its own medical documentation and can be rated separately when the causal relationship to service-connected cervical radiculopathy is established.
Sleep disruption becomes particularly problematic because cervical nerve pain often worsens when lying down. Veterans might find themselves sleeping in chairs or using multiple pillows to find comfortable positions, leading to chronic sleep deprivation and its associated health impacts.
Veterans experiencing sleep problems related to their cervical radiculopathy should understand VA ratings for insomnia as a potential secondary condition that can add to overall disability compensation.
Lumbar Radiculopathy VA Rating
Lumbar radiculopathy represents one of the most common conditions among veterans, affecting lower extremity function and often requiring comprehensive evaluation of multiple body systems due to the complex nature of lower back nerve involvement and its widespread functional impacts.
Lower Extremity Functional Assessment
Lumbar radiculopathy evaluation focuses on leg strength, walking ability, balance, and the impact on activities of daily living, with particular attention to sciatic nerve involvement that can cause severe functional limitations in mobility and independence.
The lower back serves as the foundation for nearly every physical activity. When lumbar nerve roots become damaged, the effects ripple through the entire lower body, affecting walking, standing, and basic mobility.
VA assessment focuses on measurable functional limitations:
- Walking distance before symptoms force rest
- Ability to stand for extended periods
- Leg strength testing in specific muscle groups
- Balance and coordination during movement
- Need for assistive devices like canes or walkers
Sciatic nerve involvement creates particularly disabling symptoms because this large nerve controls major leg muscles and sensation. L5-S1 radiculopathy can cause foot drop, making normal walking patterns impossible without assistive devices.
VA examiners observe gait patterns, noting any limping, shortened stride length, or compensatory movements. They also test ability to walk on heels and toes, which reveals specific nerve dysfunction patterns.
Bilateral Lumbar Radiculopathy Considerations
When lumbar radiculopathy affects both legs, the VA must consider bilateral factors and may assign separate ratings for each affected extremity, potentially resulting in higher overall disability percentages through bilateral factor calculations.
Bilateral lumbar radiculopathy creates some of the most disabling conditions veterans face. When both legs are affected by nerve damage, mobility becomes severely compromised, and the VA rating system provides additional compensation through bilateral factors.
Establishing distinct nerve involvement on both sides becomes important, not just generalized back pain. This requires:
- Imaging showing bilateral nerve compression
- Neurological testing demonstrating dysfunction in both legs
- Functional limitations affecting both lower extremities
- Documentation of bilateral symptom patterns
Bilateral lumbar radiculopathy often results from central spinal stenosis or disc herniations that compress multiple nerve roots simultaneously. The functional impact can be devastating—walking when both legs have weakness, numbness, and unpredictable pain creates severe limitations.
The bilateral factor calculation can significantly increase overall disability ratings. Two 30% ratings for bilateral lumbar radiculopathy don’t just combine to 51%—the bilateral factor pushes the combined rating higher, potentially reaching 60% or more.
Associated Spinal Conditions
Lumbar radiculopathy often occurs alongside spondylosis, degenerative disc disease, or spinal stenosis, requiring careful evaluation to determine appropriate ratings for each condition without pyramiding symptoms or double-counting functional limitations.
Spinal conditions rarely occur in isolation. Lumbar radiculopathy likely coexists with other degenerative changes that can be rated separately if they cause distinct functional limitations.
Common associated conditions include:
- Degenerative disc disease causing mechanical back pain
- Spinal stenosis creating neurogenic claudication
- Spondylosis with joint dysfunction
- Facet joint arthritis causing stiffness
- Muscle spasm and myofascial pain
The challenge lies in separating overlapping symptoms to avoid pyramiding—the VA won’t rate the same functional limitation twice under different diagnostic codes. However, if each condition causes distinct problems, separate ratings are possible.
For example, degenerative disc disease might cause mechanical back pain and stiffness, while radiculopathy causes leg weakness and numbness. These represent different functional limitations that can be rated separately.
Obtaining medical opinions that clearly distinguish between mechanical spinal problems and neurological radiculopathy symptoms becomes important. Physicians need to explain how each condition contributes to the overall disability picture.
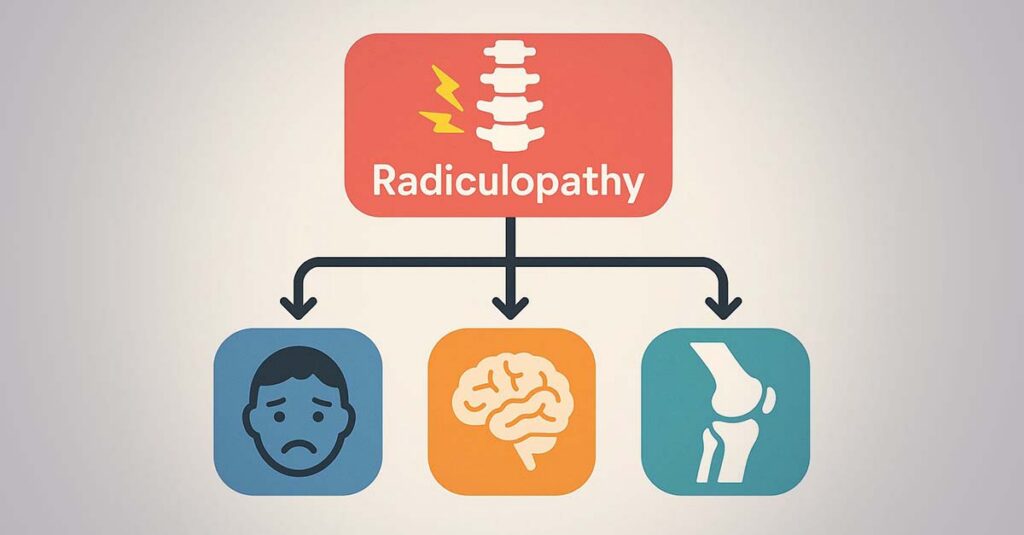
Comorbid Conditions and Secondary Service Connection
Radiculopathy frequently leads to or occurs alongside other medical conditions, creating opportunities for additional VA ratings through secondary service connection. Understanding these relationships is important for comprehensive disability compensation, as chronic nerve conditions often trigger a cascade of related health problems that can significantly impact overall quality of life and functional capacity.
VA Secondary Conditions to Radiculopathy
Many conditions can develop as a direct result of radiculopathy, including musculoskeletal compensations, psychological impacts, and medication-related side effects that may qualify for secondary service connection, potentially adding substantial disability percentages to overall ratings.
Musculoskeletal Secondary Conditions
Chronic pain and altered movement patterns from radiculopathy can lead to secondary joint problems, muscle atrophy, and postural abnormalities that warrant separate VA ratings when properly documented and linked to the primary nerve condition.
When living with chronic radiculopathy, the body develops compensatory movement patterns that eventually damage other structures. These aren’t just minor aches—they’re legitimate medical conditions that can be service-connected as secondary to radiculopathy.
Gait changes when one leg is weak or painful. Favoring the unaffected side can lead to hip problems, knee strain, or ankle issues. Over months and years, these compensations cause structural damage that requires separate medical attention.
Upper extremity radiculopathy creates similar problems. If the right arm is weak from cervical nerve damage, overusing the left arm for daily tasks can lead to:
- Shoulder impingement syndrome
- Elbow tendinitis
- Wrist strain and carpal tunnel symptoms
- Neck muscle spasm from altered posture
Each of these conditions can be rated separately when the causal connection to service-connected radiculopathy is established. Obtaining medical opinions that explain how nerve conditions led to these secondary problems becomes important.
Muscle atrophy represents another significant secondary condition. When nerves don’t function properly, the muscles they control begin to waste away. This atrophy can be measured and rated separately from the underlying nerve condition.
Secondary Conditions Tracking Template:
- Primary Condition: ________________
- Date of Service Connection: ________________
- Secondary Condition 1: ________________
- Onset Date: ________________
- Medical Opinion Obtained: Yes ☐ No ☐
- Secondary Condition 2: ________________
- Onset Date: ________________
- Medical Opinion Obtained: Yes ☐ No ☐
Psychological Impact and Mental Health
Chronic pain from radiculopathy often results in depression, anxiety, and sleep disorders that can be service-connected as secondary conditions, significantly impacting overall disability ratings and recognizing the profound psychological toll of persistent nerve pain.
Chronic nerve pain doesn’t just hurt physically—it fundamentally changes mental health. The constant discomfort, sleep disruption, and functional limitations create conditions for psychological problems that deserve recognition and compensation.
Depression commonly develops when radiculopathy limits ability to work, exercise, or enjoy activities. Veterans aren’t just dealing with physical pain—they’re grieving the loss of former capabilities and independence.
Sleep disorders become inevitable when nerve pain worsens at night. Finding comfortable positions becomes impossible, leading to chronic sleep deprivation that affects every aspect of life. Poor sleep makes pain worse, creating a vicious cycle that’s difficult to break.
Anxiety often develops around movement and activity. Veterans become fearful of triggering pain flares, leading to activity avoidance that further weakens the body and worsens the condition.
The VA recognizes these psychological impacts as legitimate secondary conditions. Mental health evaluations documenting how radiculopathy directly contributed to psychological symptoms are necessary. The timeline matters—mental health problems should have developed after nerve conditions, not before.
An Army veteran with service-connected lumbar radiculopathy developed severe depression two years after his initial rating. His chronic sciatic pain prevented him from participating in family activities and forced early retirement from his law enforcement career. A psychiatrist documented that his depression was directly caused by the functional limitations and chronic pain from his radiculopathy. The VA ultimately assigned an additional 50% rating for depression as a secondary condition.
Veterans experiencing depression related to their chronic radiculopathy should understand VA rating criteria for depression to maximize their secondary condition compensation.
Spondylosis with Radiculopathy
When spondylosis occurs with radiculopathy, the VA must carefully evaluate whether to rate these as separate conditions or as a single condition with combined symptoms, affecting the overall disability percentage and requiring strategic approaches to maximize appropriate compensation.
| Diagnostic Code | Condition | Maximum Rating | Key Evaluation Criteria |
| 5242 | Degenerative Arthritis of Spine | 100% | Range of motion, ankylosis |
| 8520 | Incomplete Paralysis of Sciatic Nerve | 80% | Functional limitations, muscle strength |
| 5243 | Intervertebral Disc Syndrome | 100% | Incapacitating episodes, functional impact |
| 8510 | Upper Radicular Group Paralysis | 70% | Grip strength, coordination |
Combined Rating Strategies
Veterans with both spondylosis and radiculopathy may benefit from strategic approaches to rating that maximize compensation while avoiding pyramiding of symptoms, requiring careful analysis of which diagnostic codes provide the most advantageous ratings for specific symptom profiles.
Spondylosis and radiculopathy often coexist, but they represent different pathological processes that can warrant separate ratings. Spondylosis involves joint degeneration and mechanical problems, while radiculopathy involves nerve compression and neurological symptoms.
The strategic question becomes: Should separate ratings be sought for each condition, or would a single rating under a different diagnostic code provide better compensation?
Separate ratings work when:
- Spondylosis causes mechanical back pain and stiffness
- Radiculopathy causes distinct neurological symptoms
- Each condition creates different functional limitations
- Medical evidence clearly distinguishes between the two
Combined ratings might be better when:
- Symptoms overlap significantly
- A single diagnostic code captures the full disability picture
- The combined approach yields a higher percentage
This decision requires careful analysis of specific symptoms and the available diagnostic codes. Sometimes a 40% rating under one code provides better compensation than two 20% ratings that combine to 36%.
Diagnostic Code Selection
Choosing the most advantageous diagnostic code requires understanding how the VA evaluates combined spinal conditions and their functional impacts, as different codes may provide varying levels of compensation for similar symptom presentations.
The VA offers multiple diagnostic codes for spinal conditions, and choosing the right one can significantly impact disability percentages. Veterans aren’t locked into the first code assigned—changes can be requested if different codes better represent conditions.
Common diagnostic codes include:
- 5242 for degenerative arthritis of the spine
- 8520 for incomplete paralysis of the sciatic nerve
- 5243 for intervertebral disc syndrome
Each code has different rating criteria and maximum percentages. Some focus on range of motion limitations, others on neurological symptoms, and some on functional capacity.
Matching specific symptoms and limitations to the diagnostic code that provides the most accurate and advantageous rating becomes important. This often requires working with medical professionals who understand VA rating criteria and can document conditions appropriately.

Navigating the VA Claims Process for Radiculopathy
Successfully obtaining an accurate VA rating for radiculopathy requires understanding the claims process, gathering appropriate evidence, and ensuring proper medical documentation that clearly demonstrates the condition’s impact on daily functioning.
Steps for Filing Radiculopathy Claims
The VA claims process for radiculopathy involves specific steps that veterans must follow to establish service connection and secure appropriate disability ratings, from initial claim preparation through final rating decisions.
Initial Claim Preparation
Veterans must gather service medical records, current medical evidence, and lay statements that establish the timeline and progression of radiculopathy symptoms from military service to present, creating a comprehensive foundation for disability claims.
Building strong radiculopathy claims starts long before filing paperwork. Constructing a compelling narrative that connects military service to current nerve conditions through solid evidence and documentation is necessary.
Starting with service medical records is important. Looking for any documentation of back injuries, neck problems, or neurological symptoms during military service matters. Even minor incidents that seemed insignificant at the time can become evidence years later.
Creating detailed timelines of symptoms helps:
- When were nerve-related symptoms first noticed?
- How have symptoms progressed since leaving service?
- What treatments have been tried?
- How do symptoms affect daily activities?
Lay statements from family members, friends, and coworkers can provide powerful evidence of how conditions have changed over time. These statements should focus on specific observations about functional limitations, not general comments about pain.
Spouses might describe struggles to sleep due to nerve pain, or inability to perform household tasks requiring prolonged standing. Coworkers might note frequent needs to change positions or take breaks due to symptoms.
Medical Evidence Requirements
Strong radiculopathy claims require comprehensive medical documentation including MRI or CT imaging, nerve conduction studies, and detailed physician assessments of functional limitations that provide objective evidence of nerve dysfunction and its impact.
Medical evidence forms the backbone of any successful radiculopathy claim. Subjective symptom reports alone provide limited value—objective findings that demonstrate actual nerve dysfunction are necessary.
Essential medical evidence includes:
- MRI or CT scans showing nerve compression or spinal abnormalities
- Nerve conduction studies demonstrating slowed electrical transmission
- EMG testing revealing muscle denervation patterns
- Detailed neurological examinations documenting specific deficits
- Functional capacity evaluations measuring real-world limitations
The timing of these tests matters. Recent studies carry more weight than older ones, but historical testing can help establish the progression of conditions over time.
Treating physicians should provide detailed reports that explain not just what they found, but how those findings relate to functional limitations. Generic statements about “chronic pain” won’t suffice—specific documentation of nerve-related symptoms and their impact on daily activities is necessary.
Understanding what evidence is needed for disability claims becomes important when building comprehensive radiculopathy cases that demonstrate clear service connection and functional impact.
C&P Examination Preparation
Veterans should prepare for VA Compensation and Pension examinations by documenting daily symptoms, functional limitations, and bringing comprehensive medical records to support their claims during this critical evaluation process.
The C&P examination represents the opportunity to demonstrate the full impact of radiculopathy to a VA examiner. Preparation can make the difference between an accurate rating and an inadequate one.
Before examinations:
- Document symptoms for several weeks leading up to appointments
- Gather all relevant medical records and bring copies
- Prepare lists of medications and treatments tried
- Think about specific examples of how symptoms affect daily activities
During examinations, being honest about limitations without downplaying symptoms is important. Some veterans try to appear strong or minimize their problems, which can result in lower ratings than conditions warrant.
Describing worst days, not best ones, helps. The VA wants to understand the full scope of disability, including how symptoms fluctuate and what happens during flare-ups.
Being specific about functional limitations matters. Instead of saying “I have trouble walking,” explaining that walking only two blocks is possible before leg pain forces rest, and that canes are needed for stability on uneven surfaces, provides clearer evidence.
C&P Exam Preparation Checklist:
- ☐ Symptom diary for 2-4 weeks before exam
- ☐ Complete medical records copied and organized
- ☐ List of all medications and dosages
- ☐ Specific examples of daily limitations
- ☐ Questions about condition prepared
- ☐ Comfortable clothing for physical examination
- ☐ Transportation arranged (avoid driving if symptoms are severe)
Average VA Ratings and Expectations
Understanding typical VA ratings for radiculopathy helps veterans set realistic expectations and identify when ratings may be inadequate for their level of impairment, providing context for the range of possible disability percentages.
Rating Range Analysis
Most radiculopathy ratings fall between 10% and 40%, though severe cases with complete paralysis may warrant higher ratings under specific diagnostic codes, helping veterans understand typical compensation levels for nerve conditions.
Radiculopathy ratings cluster around certain percentages based on symptom severity and functional impact. Understanding these patterns helps evaluate whether ratings accurately reflect disability levels.
Common rating ranges:
- 10%: Mild symptoms with minimal functional impact
- 20%: Moderate symptoms affecting some daily activities
- 30%: Significant symptoms with notable functional limitations
- 40%: Severe symptoms with substantial disability
Ratings above 40% are possible but require documentation of near-complete paralysis or total functional loss in affected nerve distributions. These higher ratings are rare and typically involve catastrophic nerve injuries.
The majority of veterans with radiculopathy receive ratings between 10% and 30%. When symptoms seem more severe than ratings suggest, grounds may exist for increase claims with additional medical evidence.
Factors Affecting Rating Decisions
VA rating decisions consider symptom severity, functional impact, response to treatment, and objective medical findings, with higher ratings requiring clear documentation of significant limitations that affect employment and daily living activities.
Several factors influence how the VA rates radiculopathy, and understanding these can help in presenting stronger evidence.
Symptom severity gets measured through objective testing, not just subjective reports. Nerve conduction studies, EMG results, and imaging findings carry more weight than pain descriptions alone.
Functional impact becomes important for higher ratings. The VA wants to see how nerve dysfunction affects ability to work, perform household tasks, and maintain independence. Detailed functional capacity evaluations can provide this evidence.
Response to treatment also matters. When conservative treatments like physical therapy and medications haven’t provided significant relief, this suggests more severe underlying pathology that might warrant higher ratings.
Consistency across multiple medical sources strengthens cases. When several different physicians document similar findings and limitations, the VA is more likely to assign appropriate ratings.
Veterans who believe their current ratings are inadequate should understand how to request a VA disability rating increase to obtain proper compensation for their nerve conditions.

Specialized Rating Considerations and Advanced Topics
Certain aspects of radiculopathy rating require specialized knowledge of VA regulations, including combined ratings calculations, temporal factors, and appeals processes that can significantly impact veteran outcomes. These advanced considerations often determine whether veterans receive maximum compensation for their service-connected nerve conditions.
Combined Disability Rating Calculations
When veterans have multiple radiculopathy conditions or radiculopathy combined with other disabilities, understanding how the VA calculates combined ratings becomes important for maximizing compensation through proper application of rating mathematics and bilateral factors.
Bilateral Factor Applications
Veterans with bilateral lumbar radiculopathy or other bilateral nerve conditions benefit from the VA’s bilateral factor, which adds percentage points to the combined rating calculation, potentially increasing monthly compensation significantly through this mathematical advantage.
The bilateral factor represents one of the most misunderstood aspects of VA rating calculations, yet it can substantially increase disability compensation when applied correctly.
In practice, bilateral factors work like this: With 20% radiculopathy in the left leg and 20% in the right leg, the standard combined rating would be 36%. However, the bilateral factor adds 10% of that combined value (3.6 points), pushing the total to approximately 40%.
This might seem like a small difference, but it translates to significant monthly compensation increases over time. The bilateral factor becomes even more valuable with higher individual ratings.
Key requirements for bilateral factor application:
- The same condition must affect paired extremities
- Each side must be rated separately
- The conditions must be truly bilateral, not just one condition affecting both sides
Documentation becomes critical. Medical records need to clearly show distinct nerve involvement on both sides, not just generalized symptoms that happen to affect both legs or arms.
Temporal Rating Considerations
Radiculopathy conditions may fluctuate over time, requiring veterans to understand when and how to seek rating increases for worsening conditions, as nerve damage can progress and create additional functional limitations that warrant higher disability percentages.
Progressive Condition Documentation
Veterans must document how radiculopathy symptoms have worsened since their initial rating, requiring updated medical evidence and functional assessments to support increase claims that reflect the current severity of their nerve conditions.
Nerve conditions rarely remain static—they often worsen over time due to continued degeneration, failed treatments, or additional injuries. Recognizing when conditions have progressed enough to warrant rating increases can significantly impact compensation.
Signs radiculopathy may have worsened:
- Increased frequency or intensity of symptoms
- New areas of numbness or weakness
- Greater functional limitations in daily activities
- Need for stronger medications or additional treatments
- Development of new secondary conditions
Documenting progression requires comparing current status to conditions at the time of last ratings. This means maintaining detailed records of symptoms, treatments, and functional limitations over time.
Recent medical evidence carries the most weight for increase claims. Updated MRI scans showing worsening nerve compression, new EMG findings demonstrating increased muscle denervation, or functional capacity evaluations revealing greater limitations all support increase requests.
Flare-Up and Remission Patterns
The VA considers the frequency and severity of radiculopathy flare-ups when determining ratings, making detailed symptom logs and medical documentation of exacerbations essential for accurate ratings that reflect the variable nature of nerve conditions.
Radiculopathy symptoms often fluctuate dramatically, with periods of relative stability interrupted by severe flare-ups that can be completely disabling. The VA rating system attempts to account for these variations, but proper documentation is necessary to ensure accurate ratings.
Flare-up documentation should include:
- Frequency of severe symptom episodes
- Duration of each flare-up period
- Specific functional limitations during exacerbations
- Triggers that precipitate worsening symptoms
- Recovery time between episodes
Many veterans make the mistake of only seeking medical attention during their best periods, which can result in ratings that don’t reflect their true disability level. Medical documentation during both stable periods and flare-ups is necessary to paint a complete picture.
Emergency room visits during severe radiculopathy flare-ups can provide valuable evidence of symptom severity. These records often contain detailed descriptions of pain levels and functional limitations that support higher ratings.
Appeals and Rating Challenges
When initial VA ratings for radiculopathy are inadequate, veterans have specific appeal options that require understanding of evidence requirements and procedural timelines, with different appeal pathways offering various advantages depending on the specific circumstances of each case.
Higher-Level Review Strategies
Veterans can request higher-level reviews when they believe their radiculopathy ratings are too low, requiring clear identification of rating errors and supporting medical evidence that demonstrates the inadequacy of the initial decision.
Higher-level reviews offer a streamlined appeal option when the VA made clear errors in rating radiculopathy. This process works best when errors involve misapplication of rating criteria rather than disputes over medical evidence.
Common rating errors include:
- Using the wrong diagnostic code for conditions
- Failing to apply bilateral factors when appropriate
- Misinterpreting medical evidence or test results
- Not considering all documented symptoms and limitations
- Applying outdated rating criteria
The higher-level review process doesn’t allow new evidence, so arguments are limited to claiming that existing evidence should have resulted in higher ratings. This makes it important to identify specific procedural or interpretive errors in original decisions.
Preparing clear arguments explaining why evidence supports higher ratings is necessary. Pointing to specific medical findings, functional limitations, or rating criteria that original examiners overlooked or misinterpreted strengthens appeals.
Supplemental Claim Preparation
New medical evidence of radiculopathy progression or previously undiagnosed nerve involvement can support supplemental claims for increased ratings, offering veterans the opportunity to present additional evidence that wasn’t available during their initial claims.
Supplemental claims work when new and relevant evidence exists that wasn’t part of original claims. This could include recent medical studies, updated physician opinions, or documentation of condition progression.
Effective supplemental claim evidence includes:
- Recent imaging showing worsening nerve compression
- New EMG or nerve conduction studies
- Updated functional capacity evaluations
- Medical opinions linking secondary conditions to radiculopathy
- Documentation of failed treatments or surgical interventions
Ensuring new evidence is truly “new and relevant” is important. Simply getting another doctor to review the same old records usually won’t qualify. Evidence that provides new information about conditions or their severity is necessary.
Timing matters for supplemental claims. Filing as soon as compelling new evidence is obtained rather than waiting to gather additional documentation is advisable. Subsequent supplemental claims can always be filed if more evidence becomes available.
Appeals Decision Tree:
- New medical evidence available? → Supplemental Claim
- Clear rating error occurred? → Higher-Level Review
- Need hearing with new evidence? → Board Appeal
- Disagree with Board decision? → Court of Appeals for Veterans Claims
Veterans considering appeals should understand common reasons for low VA disability ratings to identify whether their radiculopathy cases involve correctable rating errors or require additional medical evidence.
How REE Medical Supports Veterans with Radiculopathy Claims
Understanding VA ratings for radiculopathy can be complex, requiring comprehensive medical documentation and expert evaluation to ensure accurate disability ratings. REE Medical addresses these challenges by connecting veterans with independent licensed medical professionals who specialize in VA-compliant evaluations and documentation, helping veterans obtain the thorough medical evidence necessary for proper rating decisions.
Many veterans struggle with inadequate radiculopathy ratings because their medical records don’t fully capture the extent and impact of their nerve conditions. Standard medical appointments often focus on treatment rather than disability documentation, leaving gaps in the evidence needed for accurate VA ratings.
REE Medical’s network of experienced physicians understands the specific documentation requirements for VA radiculopathy claims. These independent medical evaluations, including Disability Benefits Questionnaires (DBQs), provide detailed medical evidence that clearly demonstrates the severity and functional impact of nerve conditions.
The independent medical evaluation process focuses on:
- Comprehensive neurological examinations documenting specific deficits
- Detailed functional assessments measuring real-world limitations
- Clear medical opinions linking symptoms to service-connected conditions
- Proper documentation of secondary conditions and their relationships
- VA-compliant reporting that addresses all relevant rating criteria
REE Medical’s compliance framework ensures complete neutrality and transparency while adhering to federal regulations (38 U.S.C. §§ 5901–5905). The company’s role is strictly limited to coordinating independent, objective medical evaluations and documentation—never filing claims, guaranteeing outcomes, or advocating for specific results.
For veterans struggling with inadequate VA ratings for radiculopathy or those seeking initial service connection, REE Medical’s complimentary consultation process helps explain how independent medical evaluations can strengthen claims.
Veterans can learn more about coordinating VA-compliant DBQs and independent medical evaluations by contacting REE Medical for an informational consultation. REE Medical’s team explains the documentation coordination process and connects veterans with independent, licensed medical providers.
Understanding the VA DBQ process helps clarify how independent medical evaluations provide the detailed evidence needed for accurate disability ratings.
Final Thoughts
Navigating VA ratings for radiculopathy requires understanding both the medical complexity of nerve conditions and the specific criteria the VA uses to evaluate disability compensation. Veterans who invest time in understanding rating principles, gathering comprehensive medical evidence, and properly documenting their functional limitations position themselves for more accurate ratings that truly reflect their service-connected disabilities.
The foundation of any successful radiculopathy claim rests on thorough medical documentation that tells the complete story of the condition and its impact on daily life. The key to success lies in building strong medical evidence that clearly demonstrates how radiculopathy impacts daily functioning, while understanding the various pathways for maximizing compensation through proper application of rating criteria, bilateral factors, and secondary condition claims.
Whether filing initial claims or seeking to increase existing ratings, comprehensive medical evidence, proper preparation, and strategic timing all contribute to maximizing chances of receiving appropriate compensation for service-connected nerve conditions.

Disclosure
DISCLAIMER: REE Medical, LLC is not a Veterans Service Organization (VSO) or a law firm and is not affiliated with the U.S. Veterans Administration (“VA”). Results are not guaranteed, and REE Medical, LLC makes no promises. REE Medical’s staff does not provide medical advice or legal advice, and REE Medical is not a law firm. Any information discussed, such as, but not limited to, the likely chance of an increase or service connection, estimated benefit amounts, and potential new ratings, is solely based on past client generalizations and not specific to any one patient. The doctor has the right to reject and/or refuse to complete a Veteran’s Disability Benefit Questionnaire if they feel the Veteran is not being truthful. The Veteran’s Administration is the only agency that can make a determination regarding whether or not a Veteran will receive an increase in their service-connected disabilities or make a decision on whether or not a disability will be considered service-connected. This business is not sponsored by, or affiliated with, the United States Department of Veterans Affairs, any State Department of Military and Veterans Affairs, or any other federally chartered veterans service organization.