Understanding VA Disability Benefits: A Comprehensive Overview for Veterans
The Veterans Benefits Administration provided more than $112 billion in disability benefits to approximately 5.4 million veterans and their families in fiscal year 2022, representing one of the largest benefit programs in the federal government. This substantial system serves veterans whose health was affected during military service, yet understanding its complexities requires careful examination of how the VA evaluates and assigns disability ratings.
This comprehensive overview explains how VA disability benefits function, what the VA evaluates when reviewing claims, and how medical documentation supports accurate assessment of service-connected conditions. Whether exploring initial claims or understanding the review process, this resource provides factual information about how the VA disability system operates.
TL;DR: Key Facts About VA Disability Benefits
- Service connection requires three elements: current diagnosed disability, in-service event or injury
- The VA uses a standardized rating schedule with 10% increments, and combined ratings follow “VA math” rather than simple addition
- Multiple claim types exist (initial, increase, secondary, supplemental) each serving different purposes within the VA system
- Medical evidence quality directly impacts how the VA evaluates claims – comprehensive documentation allows for more accurate assessment
- Compensation and Pension (C&P) examinations significantly influence ratings and represent a key part of the VA’s evaluation process
- According to the VA, veterans who disagree with decisions may request Higher-Level Review or appeal to the Board of Veterans’ Appeals within specific timeframes
- Benefits extend beyond monthly compensation to include healthcare access, vocational rehabilitation, and dependent allowances
- Understanding how the VA evaluates evidence helps veterans work with medical providers to develop thorough documentation
Understanding the VA Disability System
The VA disability system operates as a compensation framework that provides monthly payments to veterans whose injuries or illnesses stem from military service. This system assigns ratings from 0% to 100% in 10% increments, with higher percentages corresponding to increased monthly compensation and expanded benefit eligibility. Understanding how this system functions allows veterans to better comprehend what the VA evaluates when reviewing disability claims.
Analysis of fiscal year 2010 through 2020 data reveals that Non-Hispanic Black veterans had the lowest approval rates among all racial and ethnic groups at 61% versus 75% for White veterans, highlighting significant disparities in the disability compensation system that the VA continues to work to address.

The Foundation of VA Disability Claims
Service connection forms the bedrock of every VA disability rating, requiring clear evidence linking current medical conditions to military service. This connection isn’t assumed by the VA – it must be demonstrated through specific evidence and documentation that meets VA standards. Without establishing service connection, the severity of a condition alone won’t result in compensation.
Service connection depends on proof of three distinct elements working together:
- Current diagnosed disability – A medical diagnosis documented by healthcare providers showing the condition exists today
- In-service event, injury, or exposure – Documentation showing something occurred during military service
- Medical nexus – A medical professional’s opinion connecting the current condition to the military service event
The nexus requirement represents a critical element that veterans sometimes overlook. Having a current condition and remembering an event during service isn’t sufficient by itself. Medical professional opinion stating the current condition is “at least as likely as not” related to military service is typically necessary.
Establishing Service Connection
The three-element framework for service connection requires methodical documentation. Veterans working with their healthcare providers can focus on developing evidence for each element, understanding that all three must be present for the VA to establish service connection.
Current diagnosed disability means formal medical documentation of the condition exists. Healthcare provider documentation clearly stating the diagnosis and its impact on functioning provides this element.
In-service events require documentation proving something happened during military service. This could be medical records showing treatment received during service, incident reports, or statements from fellow service members who witnessed events or injuries.
Medical nexus represents the connection between the current condition and military service. Medical professional opinion linking the current condition to military service, expressed in terms the VA recognizes, provides this element. These opinions are typically based on review of medical evidence and service history.
Example: Consider a veteran experiencing chronic knee pain who injured their knee during a training exercise in 2018. The evidence for service connection would include: (1) Current medical records diagnosing osteoarthritis in the knee, (2) Military medical records or incident reports documenting the training injury, and (3) An orthopedic specialist’s opinion stating the current arthritis is “at least as likely as not” caused by the documented military injury. The VA would review all three elements when evaluating this claim.
The Role of Medical Evidence
Medical evidence serves as the foundation supporting disability evaluations, from establishing diagnosis to demonstrating severity and functional impact. The quality, comprehensiveness, and format of this evidence directly influences how VA decision-makers understand and rate conditions.
Comprehensive medical documentation extends beyond basic diagnosis. Records showing symptom frequency, severity, and functional limitations provide the VA with a complete picture. Treatment history, medication trials, and specialist consultations all contribute to this documentation.
Objective medical findings carry substantial weight in VA evaluations. While reported symptoms matter, measurable findings like range of motion limitations, test results, or observable symptoms provide concrete evidence the VA uses for rating purposes.
Timeline Considerations for Claims
According to the VA, the timing of disability claim submissions can significantly impact compensation through effective date assignments and retroactive benefit calculations. While the VA doesn’t impose deadlines for submitting claims, understanding how timing affects benefits helps veterans make informed decisions about when to engage with the claims process.
Filing within one year of discharge provides the most advantageous effective date – the separation date. When claims are approved with this timing, the VA calculates retroactive compensation back to the date of separation from military service.
Later submissions receive effective dates based on when claims were filed or when medical evidence shows conditions began, whichever is later. This can result in months or years of difference in the retroactive compensation calculation.
According to the VA, Intent to File forms can protect effective dates while evidence is gathered. Filing an intent to file gives one year to submit the formal claim while potentially preserving an earlier effective date.
VA Rating Schedule and Compensation
The VA rating schedule provides standardized criteria for evaluating disability severity across different body systems and conditions. This schedule translates medical findings into percentage ratings that determine monthly compensation amounts and additional benefit eligibility. Understanding how the VA assigns ratings helps veterans and their healthcare providers focus documentation on the factors the VA evaluates.
The rating schedule organizes conditions by body system, with specific criteria for each percentage level. These criteria focus on functional limitations rather than just diagnosis or pain levels. Understanding what the VA evaluates at each rating level helps frame how medical conditions are documented.
Monthly compensation amounts increase significantly at certain percentage thresholds. Veterans rated 30% or higher become eligible for additional compensation for dependents. Those rated 100% receive the highest monthly payments plus additional benefits like dental coverage.
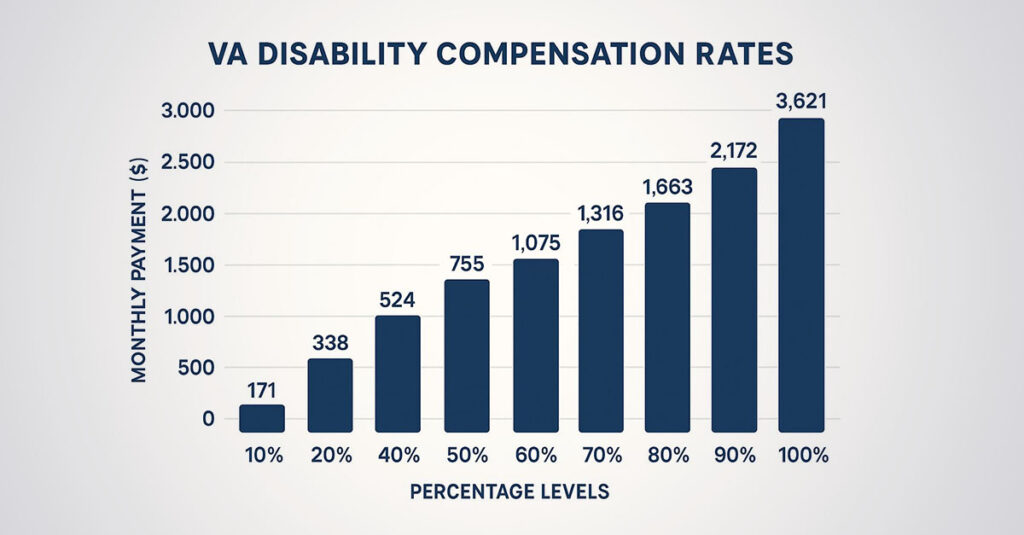
Understanding Percentage Ratings
Percentage ratings reflect the degree to which service-connected conditions impact ability to function in work and daily activities. The VA assigns these ratings based on specific criteria outlined in the rating schedule, considering factors like symptom frequency, severity, and functional limitations.
Ratings are assigned in 10% increments from 0% to 100%. A 0% rating means a veteran has a service-connected condition that doesn’t currently cause significant functional impairment according to VA criteria. Higher percentages reflect increasingly severe functional limitations as defined in the rating schedule.
Each body system has specific rating criteria. Musculoskeletal conditions might be rated based on range of motion limitations, while mental health conditions consider symptom frequency and occupational impact.
Functional limitations carry more weight than pain levels alone in VA evaluations. The VA evaluates how conditions affect ability to work, perform daily activities, and maintain relationships.
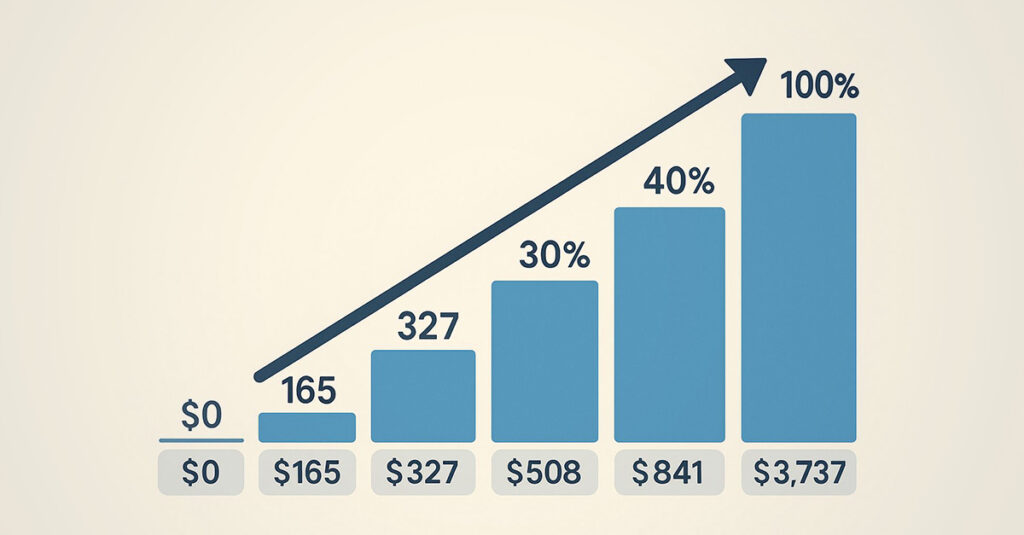
Combined Ratings Mathematics
VA mathematics for combining multiple disability ratings follows a unique “whole person” concept that often results in different combined ratings than simple addition would suggest. This system recognizes that a person can only be 100% disabled total, so each additional condition affects the remaining “efficiency” rather than adding to the full percentage.
The VA’s math starts with the highest rating and applies subsequent ratings to remaining “efficiency.” If a veteran has a 50% rating, the calculation recognizes 50% efficiency remaining. A second 30% rating applies to that remaining 50%, adding 15% (30% of 50%) for a combined 65% rating.
The VA rounds combined ratings to the nearest 10%. A calculated 64% becomes 60%, while 65% rounds up to 70%. This rounding can significantly impact monthly compensation.
Multiple lower ratings can combine to reach higher compensation levels. Three 30% ratings don’t equal 90% through simple addition, but they do combine to 66% using VA math, which rounds to 70% – a substantial compensation level.
Combined Rating Example:
| Individual Ratings | VA Math Calculation | Combined Rating |
| 50% + 30% | 50% + (30% × 50%) = 65% | 70% (rounded) |
| 40% + 30% + 20% | Complex VA calculation | 70% (rounded) |
| 70% + 50% + 30% | Complex VA calculation | 90% (rounded) |

Types of VA Disability Claims
Different claim types serve specific purposes in the VA disability system, each with unique requirements and characteristics. Veterans can submit initial claims for new conditions, increase claims for worsening disabilities, secondary claims for related conditions, or supplemental claims with new evidence. Understanding what each claim type involves helps veterans work appropriately with their healthcare providers to develop necessary documentation.
Initial Claims Process
Initial claims establish service connection for conditions never previously rated by the VA, requiring comprehensive evidence packages that demonstrate all three elements of service connection. These claims set important precedents and establish effective dates that can significantly impact retroactive compensation.
The first claim submitted for a condition requires the most comprehensive evidence package. Service connection is being established from the beginning, so every piece of documentation becomes part of the VA’s review. Medical records, service documentation, and nexus evidence all work together to present the case.
Initial claims establish important effective dates for compensation. The timing and completeness of these initial submissions can affect the calculation of retroactive benefits when the VA approves claims.
Comprehensive medical evidence becomes crucial for initial claims. The VA needs to understand current conditions, their severity, and how they connect to military service. Complete evidence packages support more efficient VA review and decision-making.
Increase Claims Strategy
Increase claims allow veterans to seek higher ratings for existing service-connected conditions that have worsened over time. These claims require new medical evidence demonstrating increased severity and functional impact compared to previous ratings.
Worsening service-connected conditions may warrant increase claims when symptoms become more severe or frequent. Current medical evidence showing conditions have deteriorated since the last rating decision supports these claims.
New medical evidence must demonstrate increased functional limitations. The VA evaluates how increased symptoms affect daily activities and work capacity, not just subjective reports of increased pain.
The VA reviews the entire condition when evaluating increase claims. Current evidence forms the basis of the VA’s assessment, which could result in a rating that’s higher, lower, or unchanged depending on what current medical evidence shows.
Secondary Claims Approach
Secondary claims create additional compensation opportunities by establishing that one service-connected condition causes or aggravates another condition. These claims require medical nexus evidence linking the primary service-connected condition to the secondary condition being claimed.
One service-connected condition causing another creates opportunities for secondary service connection. A service-connected back condition might cause depression, or service-connected PTSD might lead to sleep disorders. Medical documentation of these connections can result in additional compensation.
Medical nexus evidence remains crucial for secondary claims. Healthcare provider opinions stating the primary service-connected condition caused or aggravated the secondary condition provide the foundation the VA needs to evaluate these claims. The connection must be medically sound and well-documented.
Secondary claims can increase combined ratings substantially. Adding secondary conditions to existing service-connected disabilities often results in higher compensation brackets through VA math calculations.
Example: A veteran with service-connected PTSD rated at 70% develops chronic insomnia and erectile dysfunction as direct results of their PTSD symptoms and medications. The VA would review medical nexus evidence linking these conditions to the primary PTSD diagnosis. If the VA establishes secondary service connection for both conditions, the combined rating calculation could potentially result in an overall rating of 90% or 100% depending on the individual ratings assigned to each condition.

Supplemental Claims Options
According to the VA, supplemental claims provide opportunities to pursue previously denied claims by submitting new and relevant evidence that wasn’t available during the original decision. These claims don’t require starting the entire process over and can be submitted at any time when new evidence becomes available.
Previously denied claims can be reconsidered with new and relevant evidence. This evidence must be something that wasn’t available or considered during the original decision. New medical opinions, additional service records, or updated medical examinations can all qualify as new and relevant evidence.
Supplemental claims can maintain effective dates from original claims if successful. Rather than resetting to the new filing date, the VA may preserve the effective date from the original claim, which can result in substantial retroactive compensation for claims that were initially denied.
New evidence must be relevant to the specific reasons claims were denied. If a claim was denied for lack of medical nexus, new nexus evidence would be relevant. Additional evidence about symptom severity might not address the specific deficiency if service connection was the issue.
The Claims Review Process
Understanding the VA’s claims review procedures helps veterans know what to expect throughout the process. The VA follows specific procedures for evaluating evidence, conducting examinations, and making rating decisions. Veterans who understand these procedures can work more effectively with healthcare providers to develop documentation that aligns with what the VA reviews.
Recent controversy surrounding VA disability benefits has led to strong responses from veteran advocacy organizations. The Veterans of Foreign Wars emphasized that “veterans’ disability benefits are not charity” but rather “compensation owed for injuries and conditions incurred in the line of duty,” defending the legitimacy of the system against accusations of widespread fraud.
The Role of Medical Documentation
Thorough documentation forms the foundation of how the VA evaluates disability claims, directly impacting processing times and decision outcomes. Medical evidence that comprehensively addresses the VA’s evaluation criteria supports more efficient review and accurate assessment.
According to the VA, comprehensive claim documentation typically includes:
- Complete military service records
- Relevant medical records from service and post-service treatment
- Current medical evaluations and diagnoses
- Statements from fellow service members (buddy statements) when applicable
- Personal statements describing in-service events
- Medical nexus opinions from qualified providers
- Intent to File form (if applicable for effective date considerations)

Service Medical Records
Military medical records provide essential evidence of in-service treatment and injuries, establishing foundation evidence for service connection. These records document medical care received during military service and can demonstrate that injuries or illnesses began during service.
Service medical records contain evidence of in-service treatment, injuries, and medical conditions. These records show the VA that something happened during military service that relates to current disability claims.
Obtaining complete service medical records takes time. Records can be requested through the National Personnel Records Center, but processing can take months. Having these records available before submitting claims can prevent delays in VA processing.
Service medical records might contain evidence veterans don’t remember. Routine sick call visits, injury reports, or medical evaluations from years past can provide crucial evidence for establishing service connection.
Independent Medical Evaluations
Independent medical evaluations from qualified healthcare providers can provide detailed assessments that complement VA examinations. These evaluations offer veterans more control over the examination process and often result in more thorough documentation of conditions and their functional impacts.
Independent medical evaluations allow veterans to choose providers, schedule appointments at convenient times, and ensure adequate time for thorough evaluation. Unlike VA-scheduled examinations, these evaluations operate on the veteran’s timeline.
Qualified providers who understand VA disability requirements can provide evaluations that align with rating criteria. These providers know what information the VA evaluates and can document conditions in ways that address VA review standards.
Independent evaluations can supplement VA examinations when needed. When C&P exams are rushed or incomplete, independent evaluations can provide the thorough assessment that supports comprehensive VA review.
The VA Examination Process
VA Compensation and Pension (C&P) examinations represent critical points in the claims process, where medical professionals assess conditions and their functional impacts. These examinations directly influence rating decisions, making understanding of the process important for veterans.
In August 2024, 2.7 million veterans with service-connected disabilities were employed, with 36.5 percent working in federal, state, or local government. This demonstrates that disability ratings reflect functional limitations that impact daily life, not necessarily the ability to work in all capacities.
Understanding C&P Examinations
The VA may schedule Compensation & Pension examinations to evaluate conditions. These examinations allow VA-contracted medical professionals to assess current diagnoses, symptom severity, and functional limitations.
C&P examinations serve multiple purposes in the VA’s review process. They provide current medical assessments of conditions, document functional limitations, and help the VA understand how conditions affect daily activities and work capacity.
The format and content of C&P examinations vary depending on what conditions the VA is evaluating. Mental health examinations focus on symptom frequency and occupational impact, while musculoskeletal examinations emphasize range of motion and functional limitations.
Different conditions have different examination requirements under VA procedures. Understanding what examiners will assess helps veterans communicate effectively about their conditions’ impacts.
Veterans attending C&P examinations can bring relevant medical records and documentation. While examiners should have access to VA files, having personal copies ensures important information is available during the examination.
C&P Examination Considerations:
- The VA schedules examinations based on what evidence is needed to evaluate claims
- Examinations typically last 20-45 minutes depending on complexity
- Examiners assess current symptoms and functional limitations
- Results are documented in reports that become part of VA files
- Veterans can request copies of examination reports after completion
Understanding Examination Reports
C&P examination reports directly influence VA rating decisions. These reports translate medical conditions into the language and format that VA raters use to assign disability percentages.
Examination reports become part of VA files and inform rating decisions. These reports document findings in standardized formats that VA raters reference when applying rating schedule criteria.
Veterans can review examination reports once they become available. Reviewing these reports for accuracy in symptom documentation, functional limitations, and examiner conclusions helps veterans understand what information the VA has available when making decisions.
According to the VA, when examination reports contain errors or omissions, veterans can submit additional medical evidence to supplement the record. New medical evidence or requests for additional examinations can address deficiencies when reports don’t accurately reflect conditions.
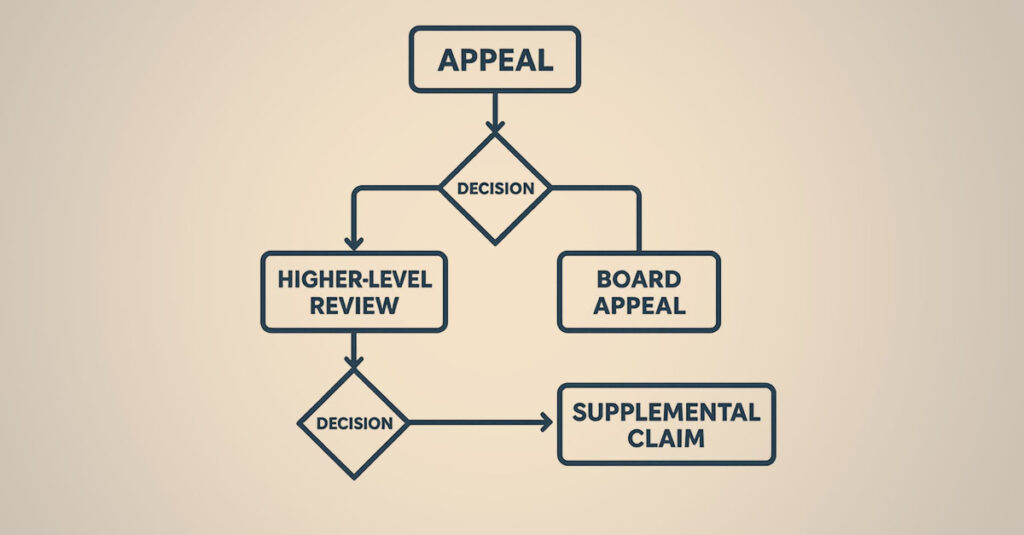
Reviews and Appeals
When initial claim decisions are unfavorable, according to the VA, veterans have multiple review options within specific timeframes. The review process provides opportunities to present additional evidence, request senior-level examination of decisions, or seek independent review.
Higher-Level Review Process
According to the VA, Higher-Level Review allows a senior VA reviewer to examine claims without considering new evidence, focusing specifically on whether original decision-makers made errors in applying VA regulations or interpreting existing evidence.
Higher-Level Review focuses on whether original decisions properly analyzed evidence that was in files. This option works when veterans believe the VA had adequate evidence but may have made errors in analysis or application of regulations.
No new evidence can be submitted during Higher-Level Review. The senior reviewer only examines evidence that was available during original decisions. When new evidence exists, other review options might be more appropriate.
Higher-Level Review typically processes faster than other review options according to VA data. Since no new evidence is considered and no hearings are held, these reviews often complete within several months.
Board of Veterans’ Appeals
According to the VA, the Board of Veterans’ Appeals provides independent review by Veterans Law Judges who weren’t involved in original claim decisions. These judges can consider new evidence and hold hearings depending on which appeal track is selected.
The VA offers three Board appeal tracks: Direct Review (fastest, no new evidence), Evidence Submission (allows new evidence), and Hearing (includes personal hearing with the judge). Each track serves different purposes depending on the circumstances of individual cases.
Board appeals take longer to process than other review options but offer the most comprehensive review. While processing times can extend significantly, Board decisions carry substantial weight in the VA system.
Understanding Your Benefits
Strategic understanding of how disability benefits function can significantly impact overall compensation and quality of life. Veterans who comprehend both the immediate and long-term implications of the VA disability system often achieve better outcomes than those who approach the process without full understanding.
The Disabled American Veterans organization recently noted that “rising number of veterans receiving VA disability compensation isn’t a story about widespread abuse or fraud; It’s a story about our nation’s continuing efforts to keep the promise,” emphasizing that increased claims are driven primarily by the PACT Act and recognition of previously ignored conditions.
Understanding Claim Priorities
Timing, sequencing, and documentation strategies can impact both individual ratings and combined disability percentages. Understanding how different approaches affect effective dates, combined ratings, and future claim opportunities helps veterans make informed decisions about when and how to work with healthcare providers to develop medical documentation.
Conditions most likely to receive significant ratings based on clear evidence and substantial functional impacts form important foundations for combined rating calculations. A single higher rating creates a base that makes additional ratings more valuable through VA math calculations.
Major conditions frequently cause or aggravate other conditions, creating opportunities for secondary claims. PTSD, significant injuries, and chronic conditions often have connections to other health issues that may warrant separate evaluation by the VA.
Example: A veteran with clear evidence of service-connected PTSD could see that condition evaluated first by the VA. Mental health conditions often receive ratings ranging from 30-100% depending on severity and functional impact. Once established at 70%, the veteran could then work with healthcare providers to document secondary conditions like sleep disorders, erectile dysfunction, and depression caused by the PTSD. The VA’s review of these secondary claims with proper medical nexus evidence could potentially result in a combined rating of 90-100% depending on individual ratings assigned to each condition.
Healthcare and Additional Benefits
VA disability benefits extend far beyond monthly compensation, encompassing healthcare access, vocational rehabilitation, educational benefits, and dependent allowances. Veterans who understand and access these additional benefits often receive value that exceeds monthly compensation payments.
Among veterans with service-connected disabilities, 35.1% have a disability rating of 50% or higher. Those with ratings of 50% or higher have significantly different employment patterns than those with ratings of 0-40%, highlighting the comprehensive nature of disability-related functional limitations.

Healthcare Benefits Integration
Service-connected veterans receive priority healthcare access through the VA system, including specialized treatment programs and services specifically designed for their conditions. This healthcare access often provides value that exceeds monthly compensation, particularly for veterans with complex or chronic conditions requiring ongoing treatment.
Service-connected veterans receive priority access to VA healthcare, often with reduced or eliminated copayments for treatment related to service-connected conditions. This healthcare access can provide tremendous value beyond monthly compensation amounts.
Specialized treatment programs exist for many service-connected conditions. PTSD programs, pain management clinics, and rehabilitation services provide targeted care that addresses the specific needs of disabled veterans.
VA healthcare integrates with disability ratings, providing continuity between compensation and treatment. Service-connected conditions receive priority treatment, and healthcare records maintained within the VA system can support future increase claims when conditions worsen over time.
Vocational Rehabilitation Opportunities
According to the VA, Chapter 31 Vocational Rehabilitation and Employment benefits provide education, training, and employment assistance for veterans whose service-connected disabilities impact ability to work in previous occupations. These benefits can include full tuition coverage, monthly housing allowances, and comprehensive support services that help veterans transition to new careers.
Chapter 31 benefits provide education, training, and employment assistance when service-connected disabilities affect work capacity. These benefits can be more valuable than GI Bill benefits for eligible veterans depending on individual circumstances.
Vocational rehabilitation covers full tuition, provides monthly housing allowances, and includes support services like career counseling and job placement assistance. The program focuses on helping veterans achieve employment in suitable occupations given their service-connected limitations.
According to the VA, employment handicap determinations consider how service-connected conditions affect ability to work in previous occupations. Veterans rated 20% or higher may qualify if their disabilities create employment challenges.

Common Documentation Challenges
Veterans frequently encounter specific obstacles related to evidence development and documentation, but understanding these challenges enables proactive approaches to addressing them effectively. Common issues include insufficient medical evidence, missing service records, and gaps in documentation that the VA needs to evaluate claims thoroughly.
Evidence Development Considerations
Insufficient or inadequate medical evidence represents the most common reason the VA cannot fully evaluate claims or assigns lower ratings than expected. Veterans often face challenges obtaining comprehensive medical evaluations, establishing medical nexus, or presenting evidence in formats that align with VA requirements.
Addressing Gaps in Medical Records
Missing or incomplete service medical records can be supplemented through alternative evidence sources. Personal statements, statements from fellow service members, and independent medical opinions can help establish service connection even when official records are incomplete or missing.
Missing service medical records don’t automatically prevent the VA from establishing service connection. Alternative evidence sources can fill gaps when official documentation is incomplete or missing.
Statements from fellow service members who witnessed injuries or observed symptoms can provide evidence the VA considers. These statements carry weight when they’re detailed and specific about what witnesses observed during military service.
Personal statements describing in-service experiences, injuries, and symptoms can supplement missing medical records. While not as strong as official documentation, detailed personal accounts can support service connection when combined with other evidence.
Independent medical opinions can bridge gaps between missing service records and current conditions. Qualified medical professionals can review available evidence and provide nexus opinions even when service medical records are incomplete.
Addressing Inadequate C&P Examinations
When VA examinations are insufficient or incomplete, according to the VA, veterans can request new examinations or submit independent medical evidence to supplement the record. Insufficient C&P exams may result from time constraints, examiner unfamiliarity with specific conditions, or incomplete review of medical records.
According to the VA, inadequate C&P examinations can be addressed through several mechanisms. When examinations were clearly insufficient, requests for new examinations or submission of independent medical evidence can supplement inadequate assessments.
Documenting examination deficiencies immediately after C&P exams helps support any necessary requests for additional evaluation. Notes about whether examiners seemed rushed, unfamiliar with conditions, or failed to review important medical records can be relevant if additional examination is needed.
Independent medical evaluations can supplement VA examinations. When C&P exams are insufficient, comprehensive independent evaluations often provide the thorough assessment that supports complete VA review.
According to the VA, requests for new C&P examinations can be made when original examinations were clearly inadequate. The VA may order new examinations when there’s evidence the original exam was insufficient or when new medical evidence raises questions about previous findings.
How REE Medical Coordinates Independent Medical Documentation
At REE Medical, we understand the challenges veterans face when developing comprehensive medical evidence. Our nationwide network of experienced providers coordinates independent medical evaluations that are formatted for VA review and address common documentation gaps.
REE Medical connects veterans with qualified medical professionals who understand how conditions align with VA rating criteria. Independent evaluations coordinated through our network take the time needed to properly assess conditions and document their functional impacts. This comprehensive approach provides the medical evidence that supports thorough VA review.
Our transparent flat-rate pricing eliminates confusion about costs. Veterans know exactly what they’re paying upfront, with no hidden fees or commissions. We offer free consultations so veterans can learn more about our services and whether independent medical documentation is appropriate for their situation before making any commitments.
Whether a veteran is pursuing disability benefits for an unrated condition or needs updated documentation for a previously service-connected disability, REE Medical coordinates independent medical evaluations and Disability Benefits Questionnaires (DBQs) that the VA can consider as part of its review. Our team connects veterans with licensed medical professionals who complete independent evaluations and Disability Benefits Questionnaires (DBQs) that align with VA formatting standards.
Contact us today to schedule your free consultation and learn how REE Medical coordinates independent, VA-compliant medical evaluations.
Final Thoughts
Understanding VA disability benefits requires comprehending the system’s complexities while maintaining focus on the ultimate goal – appropriate compensation for service-connected conditions and access to benefits that support quality of life. The process demands patience and persistence, but veterans who approach their claims with thorough documentation often achieve outcomes that significantly impact their financial security and well-being.
The VA disability system, while complex, exists to serve veterans who gave so much in service to our country. Service-connected conditions deserve proper evaluation and compensation, and understanding how the VA reviews evidence helps veterans work effectively with healthcare providers to develop the documentation needed for accurate assessment.
Disclosure
DISCLAIMER: REE Medical, LLC is not a Veterans Service Organization (VSO) or a law firm and is not affiliated with the U.S. Veterans Administration (“VA”). Results are not guaranteed, and REE Medical, LLC makes no promises. REE Medical’s staff does not provide medical advice or legal advice, and REE Medical is not a law firm. Any information discussed, such as, but not limited to, the likely chance of an increase or service connection, estimated benefit amounts, and potential new ratings, is solely based on past client generalizations and not specific to any one patient. The doctor has the right to reject and/or refuse to complete a Veteran’s Disability Benefit Questionnaire if they feel the Veteran is not being truthful. The Veteran’s Administration is the only agency that can make a determination regarding whether or not a Veteran will receive an increase in their service-connected disabilities or make a decision on whether or not a disability will be considered service-connected. This business is not sponsored by, or affiliated with, the United States Department of Veterans Affairs, any State Department of Military and Veterans Affairs, or any other federally chartered veterans service organization.