VA Disability Rating for Neuropathy in Feet: Understanding How the VA Evaluates Peripheral Nerve Damage
Peripheral neuropathy in the feet is one of the most debilitating—and most commonly misunderstood—conditions in the VA disability system. Veterans often struggle with burning pain, numbness, muscle weakness, and balance issues that impact nearly every aspect of daily life.
Understanding the disability compensation calculator helps veterans estimate potential monthly benefits based on their neuropathy disability ratings.
Table of Contents
- Understanding Neuropathy and VA Disability Ratings
- Navigating the Claims Process
- Rating Schedules and Compensation Levels
- Appeals and Rating Increases
- Advanced Considerations for Neuropathy Claims
- Specific Action Steps for Veterans
- Final Thoughts
TL;DR
- Peripheral neuropathy in feet affects millions of veterans and can result from service-connected exposures, diabetes, or trauma sustained during military service
- The VA rates neuropathy primarily under Diagnostic Code 8520, focusing on functional impairment rather than just pain symptoms
- Successful claims require comprehensive medical documentation including nerve conduction studies, EMG testing, and detailed functional assessments
- Rating percentages range from 10% to 100% based on severity of muscle weakness, sensory deficits, and impact on daily activities
- Veterans with bilateral neuropathy may qualify for additional bilateral factor calculations and special monthly compensation
- The C&P examination is critical—proper preparation and post-exam documentation review can significantly impact final ratings
- Multiple appeal pathways exist for inadequate ratings, including supplemental claims and higher-level reviews
Understanding Neuropathy and VA Disability Ratings
This section establishes the foundation for understanding how peripheral neuropathy affects veterans and how the VA approaches rating this complex neurological condition. The different types of service-connected neuropathy, requirements for establishing service connection, and specific criteria the VA uses to evaluate functional impairment are explored.
What Peripheral Neuropathy Really Means for Veterans
Peripheral neuropathy represents damage to the peripheral nervous system, particularly affecting feet and lower extremities. For veterans, this condition frequently stems from diabetes, Agent Orange exposure, chemotherapy treatments, or direct trauma sustained during service—each requiring different approaches to documentation and rating.
Peripheral neuropathy isn’t just “nerve pain” (though that’s certainly part of it). When discussing neuropathy in feet, the focus is on damage to nerves that control sensation, movement, and function in lower extremities. This damage can manifest as burning pain, numbness, tingling, muscle weakness, or complete loss of sensation.
The VA recognizes that military service creates unique risks for developing neuropathy. Chemical exposures, prolonged standing, heavy equipment operation, and combat injuries all contribute to nerve damage that may not become apparent until years after service ended.

Types of Service-Connected Neuropathy
The VA recognizes several distinct categories of neuropathy, each with different causes and documentation requirements. Understanding which type applies to specific situations is important for building successful claims and obtaining appropriate diagnostic codes for rating purposes.
Diabetic peripheral neuropathy represents the most common type among veterans. When diabetes develops during or after service (particularly if connected to Agent Orange exposure), the resulting neuropathy can be service-connected. The VA has established presumptive connections for certain veterans exposed to herbicides.
Toxic neuropathy results from chemical exposure during military service. Agent Orange, burn pit exposure, and other environmental hazards can cause nerve damage that develops gradually over time. These cases often require extensive documentation linking exposure to current symptoms.
Traumatic neuropathy stems from direct injuries sustained during service—vehicle accidents, falls, crush injuries, or blast injuries that damaged nerves in feet or legs. These cases typically have clearer documentation in service medical records.
Establishing Service Connection: Foundation for Benefits
Veterans must demonstrate a clear link between their military service and the development of neuropathy through medical evidence, service records, and expert medical opinions. This process requires three key elements: a current diagnosis, evidence of an in-service event or exposure, and a medical nexus connecting the two.
Service connection forms the cornerstone of neuropathy claims. Without it, even severe symptoms won’t qualify for VA disability benefits. Three elements must be established: a current medical diagnosis of neuropathy, evidence of an in-service incident or exposure, and a medical opinion linking current conditions to military service.
Service medical records become important here. Even minor foot injuries, documented chemical exposures, or early symptoms noted during service can support claims. Sick call visits, physical therapy records, or mentions of foot problems in routine medical examinations shouldn’t be overlooked.
Medical nexus opinions often make or break neuropathy claims. A qualified physician must review service records and current medical evidence, then provide an opinion about whether neuropathy is “at least as likely as not” related to military service. For comprehensive guidance on obtaining these critical medical opinions, veterans should understand how nexus letters work for establishing service connection and their role in successful disability claims.
Current VA Rating Criteria for Neuropathy
The VA evaluates neuropathy under specific diagnostic codes, primarily focusing on functional impairment rather than subjective symptoms. Understanding these criteria helps veterans prepare appropriate medical evidence and set realistic expectations for disability ratings.
The VA doesn’t rate neuropathy based on pain experience alone. Instead, focus centers on measurable functional limitations—what can’t be done because of neuropathy. This approach requires objective medical evidence demonstrating specific impairments.
Diagnostic Code 8520 covers incomplete paralysis of the sciatic nerve and serves as the primary rating criteria for most foot neuropathy cases. However, depending on which specific nerves are affected, conditions might be rated under different codes like 8524 for peroneal nerve issues.
| Diagnostic Code | Nerve Affected | Maximum Rating | Common Symptoms |
| 8520 | Sciatic Nerve | 80% | Foot weakness, sensory loss, pain |
| 8524 | Peroneal Nerve | 40% | Foot drop, difficulty lifting foot |
| 8526 | Tibial Nerve | 40% | Plantar flexion weakness, heel numbness |
| 8540 | Femoral Nerve | 40% | Knee extension weakness, thigh numbness |
Functional Assessment Requirements That Actually Matter
Ratings are based on the degree of functional loss, including muscle weakness, sensory deficits, and impact on mobility and daily activities. The VA requires objective measurements and standardized testing to determine these functional limitations, making comprehensive medical documentation essential.
Muscle strength testing uses a standardized 0-5 scale where 5 represents normal strength and 0 indicates complete paralysis. The VA looks for documented weakness in specific muscle groups affected by neuropathy. Ankle dorsiflexion (lifting the foot up) and plantar flexion (pointing the foot down) are particularly important for foot neuropathy ratings.
Sensory testing involves documented loss of sensation to light touch, vibration, or position sense. These tests must be performed by qualified medical professionals using standardized techniques. Subjective reports of numbness aren’t sufficient—objective documentation is necessary.
Range of motion measurements become critical when neuropathy affects ability to move feet and ankles normally. Limited dorsiflexion can significantly impact walking and balance, leading to higher disability ratings.
Pain and Sensory Considerations: Why They’re Not Enough
While pain is a significant symptom of neuropathy, the VA primarily rates based on objective neurological findings and functional limitations rather than subjective pain reports alone. This approach requires veterans to focus on documenting measurable impairments rather than just describing pain levels.
Pain scales and subjective symptom reports carry less weight in VA neuropathy ratings than many expect. While pain is real and debilitating, the VA requires objective evidence of functional impairment to assign meaningful disability ratings.
Sensory deficits must be documented through standardized neurological testing. Simple statements like “patient reports numbness” won’t support higher ratings. Formal sensory testing with documented areas of decreased sensation mapped out by qualified examiners is necessary.
Translating subjective symptoms into objective functional limitations is key. When burning pain prevents walking long distances, documentation of reduced walking tolerance with specific measurements is needed.
Range of Motion and Gait Analysis: Details That Count
Comprehensive evaluations include detailed assessments of ankle dorsiflexion, plantar flexion, and overall gait stability to determine the extent of functional impairment. These measurements provide objective data that directly correlates with disability rating percentages.
Gait analysis reveals how neuropathy affects walking patterns, balance, and stability. Abnormal gait patterns due to weakness, sensory loss, or pain can significantly impact daily functioning and support higher disability ratings.
Ankle range of motion measurements must be precise and documented in degrees. Normal dorsiflexion ranges from 0-20 degrees, while plantar flexion normally reaches 0-50 degrees. Limitations in these ranges due to neuropathy can support specific rating percentages.
Balance testing becomes particularly important for neuropathy cases. Loss of proprioception (position sense) in feet can cause significant balance problems, increasing fall risk and limiting ability to perform daily activities safely.

Documentation Standards and Medical Evidence
Successful neuropathy claims require comprehensive medical documentation that clearly establishes the diagnosis, severity, and functional impact of the condition through objective testing and clinical findings. This documentation must meet specific VA standards and include particular types of evidence to support disability ratings.
Medical evidence quality often determines the difference between a 10% rating and a 60% rating for the same condition. The VA requires specific types of documentation, performed by qualified providers, using standardized testing methods.
Medical records need to paint a complete picture of how neuropathy affects daily life. Generic statements about “nerve pain” won’t suffice. Detailed documentation of specific functional limitations, objective test results, and clear diagnostic findings is necessary.
Timing matters significantly in neuropathy documentation. The VA wants to see consistent findings over time, not just a single examination. Regular follow-up appointments with documented progression or stability of symptoms strengthen claims.
Nerve Conduction Studies and EMG Testing: Objective Proof
Electrodiagnostic testing provides objective evidence of nerve damage and is important for establishing the severity and extent of neuropathy for VA rating purposes. These tests offer measurable data that supports disability claims and can differentiate between various types of nerve damage.
Nerve conduction studies (NCS) measure how fast electrical signals travel through nerves. Slowed conduction velocities or reduced amplitudes provide objective evidence of nerve damage that the VA reviews. These tests are particularly valuable because they’re completely objective—no subjective interpretation required.
Electromyography (EMG) testing evaluates muscle response to nerve stimulation, revealing whether nerve damage has progressed to affect muscle function. Abnormal EMG findings often correlate with higher disability ratings because they demonstrate functional impairment.
The timing of these tests matters. Recent testing (within the past year) carries more weight than older studies. When conditions have worsened since last electrodiagnostic testing, updated studies can support claims for rating increases.
Understanding proper documentation and evidence collection is important for any VA disability claim. Veterans should be aware of what evidence is needed for disability claims to ensure they provide comprehensive support for their neuropathy ratings.
A veteran with diabetic neuropathy underwent nerve conduction studies showing severely delayed conduction velocities in both peroneal nerves (25 m/s, normal >44 m/s) and absent sensory responses in the sural nerves. Combined with clinical findings of foot drop and sensory loss, this objective evidence supported a 40% rating for each foot under diagnostic code 8524.
Navigating the Claims Process
The VA claims process for neuropathy involves specific steps and requirements that veterans must understand to maximize their chances of receiving an accurate disability rating. This section covers the essential elements of filing initial claims, preparing for examinations, and ensuring proper documentation throughout the process.
Initial Claim Filing Steps
Filing an initial claim for neuropathy requires careful preparation of medical evidence, service records, and supporting documentation to establish both service connection and the current severity of symptoms. Proper preparation at this stage can significantly impact final ratings and reduce the need for appeals.
Filing initial neuropathy claims isn’t just about filling out forms—it’s about building compelling cases that clearly demonstrate service connection and current functional limitations. The evidence submitted initially often determines whether adequate ratings are received or years are spent pursuing appropriate compensation.
VA Form 21-526EZ serves as the primary application, but the real work lies in gathering supporting evidence. Providing comprehensive evidence upfront dramatically improves chances of success. Veterans can learn more about completing VA Form 21-526EZ properly to ensure their applications include all necessary information.
Fully developed claims (FDCs) can expedite processing time and often result in more favorable outcomes. When all necessary evidence is submitted with initial applications, the VA can make decisions without requesting additional information or scheduling multiple examinations.

Gathering Service Medical Records: Historical Foundation
Veterans need to compile comprehensive service medical records that document any foot injuries, exposures, or early symptoms of neuropathy that occurred during military service. These records provide the historical foundation for establishing service connection and may contain evidence that veterans don’t remember or initially consider relevant.
Service medical records contain the historical evidence needed to establish service connection. Even seemingly minor entries—sick call visits for foot pain, physical therapy for ankle injuries, or routine physical exam findings—can support neuropathy claims years later.
Deployment health assessments, post-deployment health reassessments, and separation physical examinations shouldn’t be overlooked. These documents often contain the first mentions of symptoms that later developed into full-blown neuropathy. Early documentation of numbness, tingling, or foot pain can be invaluable.
Unit medical records, if available, may contain additional evidence of injuries or exposures not documented in individual medical files. Combat medic treatment records, field hospital visits, or evacuation documentation can provide service connection evidence.
Obtaining Current Medical Evaluations: Present-Day Evidence
Recent medical examinations from qualified healthcare providers are essential to document the current state of neuropathy and its functional impact on veterans’ lives. These evaluations must meet specific standards and include particular types of testing to support VA disability ratings effectively.
Current medical evidence must clearly document neuropathy diagnosis, severity, and functional impact. Generic office visit notes stating “patient has neuropathy” won’t support meaningful disability ratings. Comprehensive neurological evaluations with specific findings and functional assessments are necessary.
Neurologists, physiatrists, or other specialists typically provide the most credible evaluations for neuropathy claims. While family physicians can document symptoms, specialist evaluations carry more weight in the VA rating process, particularly for complex cases.
Medical evaluations should include detailed sensory testing, muscle strength assessments, reflex examinations, and functional capacity evaluations. Providers should document specific limitations in walking, standing, balance, and daily activities caused by neuropathy.
Compensation and Pension Examinations
The C&P examination is a critical component of the neuropathy rating process, where VA examiners assess veterans’ conditions according to specific protocols and rating criteria. Understanding what to expect and how to prepare can significantly impact examination outcomes and resulting disability ratings.
The Compensation and Pension (C&P) examination often determines final disability ratings, making it one of the most important appointments veterans attend. VA examiners follow specific protocols designed to evaluate neuropathy according to rating schedule criteria.
C&P examiners are tasked with conducting objective evaluations according to VA guidelines. However, the quality and thoroughness of these examinations can vary significantly between examiners and locations.
Understanding the examination process helps in preparing effectively and ensures examiners capture all relevant information about conditions. Poor preparation can result in inadequate documentation and lower ratings than conditions warrant.
Preparing for C&P Exams: Maximizing Opportunities
Veterans should prepare by documenting daily symptoms, bringing relevant medical records, and understanding what examiners will assess during neurological evaluations. Proper preparation ensures that all relevant information about conditions’ impacts is captured during these critical examinations.
Documenting symptoms for at least two weeks before C&P exams is helpful. Keeping daily logs noting pain levels, functional limitations, medication effects, and how neuropathy impacts daily activities helps in providing specific examples during examinations.
Bringing copies of all relevant medical records, including recent specialist evaluations, diagnostic testing results, and treatment records is important. While the VA should have these documents, having copies ensures examiners can review current evidence during appointments.
Understanding what examiners will assess matters. For neuropathy, expect sensory testing, muscle strength evaluation, reflex testing, range of motion measurements, and questions about functional limitations. Knowing what to expect reduces anxiety and helps in providing complete information.
Common Examination Components: What Actually Happens
C&P exams for neuropathy typically include sensory testing, muscle strength assessments, reflex evaluations, and functional capacity measurements. Understanding these components helps veterans know what to expect and ensures they can participate fully in the examination process.
Sensory testing involves checking ability to feel light touch, vibration, and position changes in feet. Examiners may use tuning forks, monofilaments, or other tools to test sensation in different areas. Being honest about what can and cannot be felt is important—this isn’t a test to “pass.”
Muscle strength testing evaluates the power in muscles controlled by affected nerves. Examiners ask veterans to move feet and toes against resistance while they grade strength on a 0-5 scale. Trying to “power through” weakness doesn’t help—accurate assessment requires honest effort.
Reflex testing checks how nerves respond to stimulation. Diminished or absent reflexes provide objective evidence of nerve damage. Examiners test ankle reflexes and possibly others depending on specific symptoms.
Post-Examination Documentation: Protecting Interests
Following C&P exams, veterans should review examination reports for accuracy and completeness, as errors can significantly impact final rating decisions. This review process allows veterans to identify and address any discrepancies before rating decisions are finalized.
Requesting copies of C&P examination reports as soon as they’re available is important. Veterans have the right to review these documents, and errors are more common than many expect. Inaccurate documentation can significantly impact disability ratings.
Reviewing reports carefully for factual errors, missing information, or mischaracterized symptoms is necessary. When examiners document normal sensation when sensory loss was clearly demonstrated, that error needs correction.
When significant errors are identified, statements correcting the record can be submitted or new examinations can be requested. Minor errors shouldn’t be assumed irrelevant—they can be the difference between rating levels.
Rating Schedules and Compensation Levels
The VA uses specific diagnostic codes and rating criteria to assign disability percentages for neuropathy, with compensation levels ranging from 10% to 100% based on the severity of functional impairment and symptoms. Understanding these rating schedules helps veterans set realistic expectations and identify when current ratings may be inadequate for their level of impairment.

Understanding Diagnostic Codes
Neuropathy in feet may be rated under various diagnostic codes depending on the specific nerves affected and the underlying cause of the condition. Each diagnostic code has specific criteria and rating percentages, making it important for veterans to understand which code applies to their situation and how it affects their potential compensation.
The VA’s rating system for neuropathy can seem confusing because multiple diagnostic codes might apply to conditions. Specific symptoms, affected nerves, and functional limitations determine which code the VA uses—and this choice significantly impacts disability ratings.
Diagnostic Code 8520 (incomplete paralysis of the sciatic nerve) serves as the most common rating criteria for foot neuropathy. This code evaluates functional loss rather than specific nerve damage, making it applicable to various types of neuropathy affecting feet and lower legs.
Some cases require rating under multiple codes when neuropathy affects different nerve distributions or causes secondary conditions. Understanding these possibilities helps in advocating for comprehensive ratings that reflect total impairment.
Primary Diagnostic Codes for Foot Neuropathy
Common codes include 8520 for sciatic nerve paralysis, 8524 for peroneal nerve paralysis, and specific codes for diabetic neuropathy depending on the presentation. Each code has distinct criteria and rating percentages, requiring veterans to understand which applies to their specific type of nerve damage.
Code 8520 covers incomplete paralysis of the sciatic nerve and applies to most cases of foot neuropathy. Ratings under this code range from 10% to 80% based on the degree of functional impairment, muscle weakness, and sensory loss.
Code 8524 addresses peroneal nerve paralysis, which commonly causes foot drop and affects ability to lift feet upward. This condition significantly impacts walking and balance, often warranting higher disability ratings.
Diabetic neuropathy may be rated under specific endocrine codes or neurological codes depending on the presentation. Veterans with service-connected diabetes who develop neuropathy may receive separate ratings for both conditions.
Secondary Rating Considerations
Veterans may be eligible for additional ratings for associated conditions such as skin disorders, balance problems, or secondary orthopedic issues resulting from altered gait. These secondary conditions can significantly increase overall disability compensation when properly documented and claimed.
Neuropathy rarely exists in isolation—it often causes or contributes to other medical conditions that warrant separate disability ratings. Skin conditions from decreased sensation, balance disorders from proprioceptive loss, and orthopedic problems from altered gait patterns all qualify for additional ratings.
Skin ulcers or infections resulting from decreased sensation in feet can be rated separately under dermatological codes. These conditions often develop because minor injuries can’t be felt and become infected or fail to heal properly.
Balance disorders and increased fall risk from neuropathy may qualify for vestibular or neurological ratings. When neuropathy causes significant balance problems that limit mobility or increase injury risk, documenting these issues thoroughly is important.
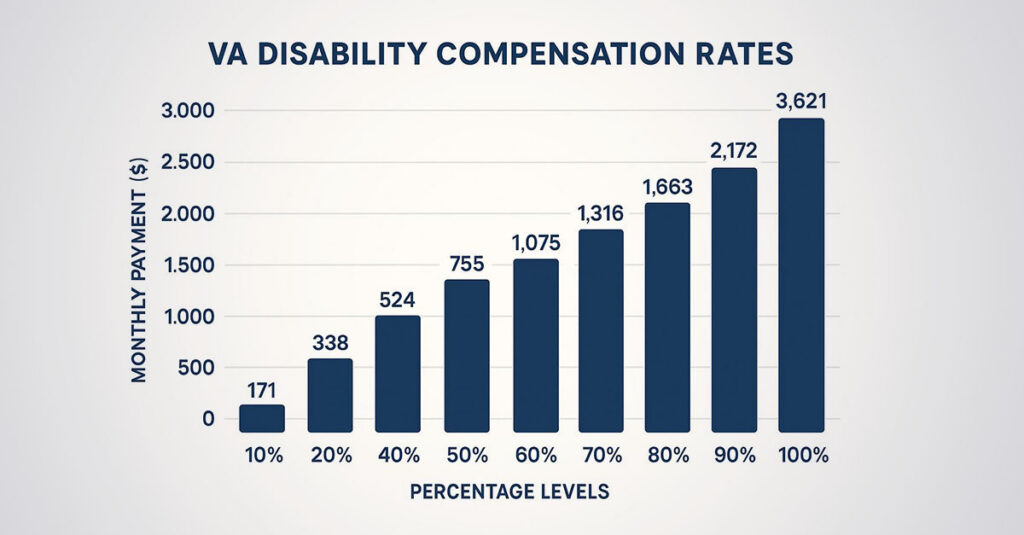
Percentage Rating Criteria
Rating percentages are assigned based on specific functional limitations and neurological findings, with higher ratings requiring more severe impairments and objective evidence. Understanding these criteria helps veterans prepare appropriate medical evidence and identify when current ratings may be inadequate.
The VA’s percentage ratings for neuropathy follow specific criteria based on functional impairment severity. These aren’t arbitrary numbers—each percentage corresponds to particular levels of muscle weakness, sensory loss, and functional limitation.
Higher ratings require more severe impairments with objective medical evidence. Simply claiming severe symptoms won’t result in high ratings without documentation supporting that level of impairment.
Understanding rating criteria helps in communicating effectively with healthcare providers about the specific documentation needed to support disability levels. Many veterans receive lower ratings because their medical records don’t adequately document the severity of their functional limitations.
10% to 30% Rating Criteria
Lower ratings typically involve mild sensory symptoms, minimal functional limitation, and preserved muscle strength with some documented neurological abnormalities. These ratings apply when neuropathy causes noticeable symptoms but doesn’t significantly impair daily functioning or work capacity.
A 10% rating typically applies when mild sensory symptoms exist with minimal functional impact. Numbness, tingling, or occasional pain might be experienced, but muscle strength remains normal and daily activities aren’t significantly affected.
20% ratings involve more noticeable sensory deficits or mild muscle weakness that causes some functional limitation. Difficulty with fine motor tasks or balance problems might occur, but major life activities remain manageable.
30% ratings require moderate sensory loss or mild to moderate muscle weakness that noticeably impacts daily functioning. Walking long distances might become difficult, or certain activities might need modification due to weakness or sensory deficits.
40% to 60% Rating Criteria
Moderate ratings require significant functional impairment, measurable weakness, and substantial impact on mobility and daily activities. These ratings reflect neuropathy that meaningfully limits ability to work and perform routine tasks, requiring comprehensive medical documentation of specific functional deficits.
40% ratings involve significant functional impairment with moderate muscle weakness and sensory loss. Difficulty walking on uneven surfaces, requiring assistive devices for longer distances, or experiencing frequent balance problems might occur.
50% ratings require marked functional limitation with considerable muscle weakness. Daily activities become challenging, work capacity is significantly reduced, and assistive devices for mobility or safety may be necessary.
60% ratings involve severe functional impairment with marked muscle weakness and extensive sensory loss. Independent mobility becomes limited, fall risk increases substantially, and many daily activities require assistance or modification.
| Rating Percentage | Functional Limitations | Muscle Strength | Sensory Loss | Daily Impact |
| 10% | Minimal | Normal (5/5) | Mild | Slight modification |
| 20% | Mild | Slight weakness (4/5) | Moderate | Some limitations |
| 30% | Moderate | Moderate weakness (3-4/5) | Significant | Notable restrictions |
| 40% | Significant | Marked weakness (2-3/5) | Extensive | Major limitations |
| 60% | Severe | Severe weakness (1-2/5) | Complete areas | Requires assistance |
| 80% | Near complete | Minimal function (0-1/5) | Total loss | Dependent care |
70% to 100% Rating Criteria
Higher ratings are reserved for severe cases with marked muscle weakness, significant functional loss, and substantial impact on ability to work and perform daily activities. These ratings require extensive medical documentation and often involve complete or near-complete loss of function in affected areas.
70% ratings require severe functional impairment with marked muscle weakness and extensive sensory loss. Independent ambulation becomes severely limited, assistive devices are necessary for safety, and work capacity is markedly reduced.
80% ratings involve near-complete functional loss with severe muscle weakness approaching paralysis. Independent mobility is severely compromised, and most daily activities require significant assistance or adaptive equipment.
100% ratings are reserved for complete functional loss equivalent to amputation. This level requires total or near-total paralysis of affected muscles with complete sensory loss, rendering affected limbs essentially non-functional.
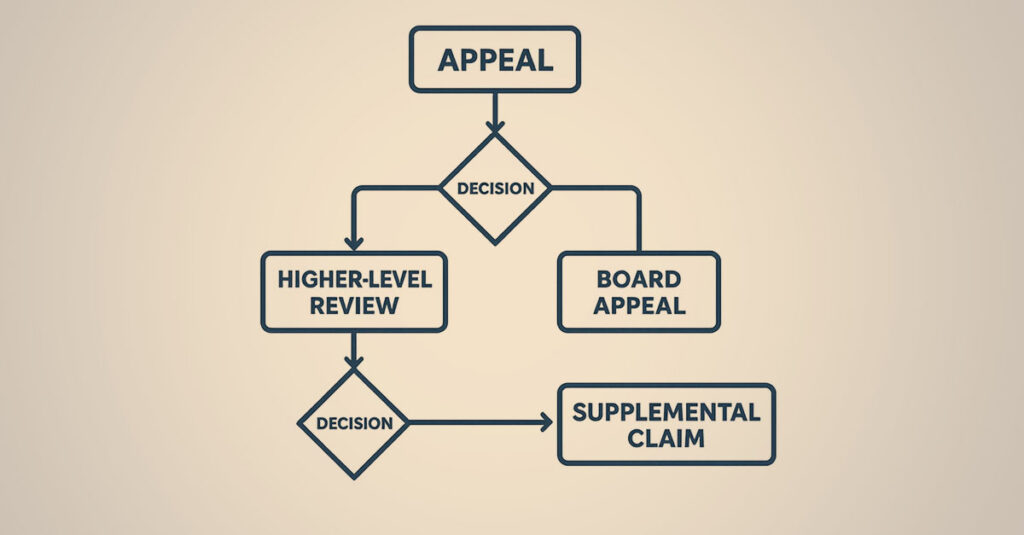
Appeals and Rating Increases
Veterans who receive inadequate initial ratings or whose conditions worsen over time have several options for appealing decisions or requesting rating increases through the VA’s established procedures. Understanding these options and when to use them can help veterans obtain disability ratings that accurately reflect their current level of impairment.
When to Consider an Appeal or Increase
Veterans should evaluate their current ratings against their actual functional limitations and consider whether new evidence or worsening symptoms justify pursuing higher ratings. This evaluation process involves comparing current symptoms with rating criteria and identifying gaps in medical documentation that may have led to inadequate ratings.
Initial disability ratings might not accurately reflect neuropathy’s true impact on life. Rating decisions sometimes miss important evidence, fail to consider all symptoms, or don’t account for bilateral involvement or secondary conditions.
Neuropathy often progresses over time, and symptoms today might be significantly worse than when initial ratings were received. Progressive conditions like diabetic neuropathy frequently worsen, warranting rating increases as functional limitations become more severe.
New medical evidence can support appeals even when symptoms haven’t changed. Better documentation of existing symptoms, additional diagnostic testing, or specialist evaluations might reveal impairments that weren’t adequately captured in original ratings.
Identifying Rating Discrepancies
Common indicators for appeal include ratings that don’t reflect current symptom severity, missing consideration of bilateral involvement, or failure to account for secondary conditions. Recognizing these discrepancies helps veterans determine when current ratings are inadequate and what evidence might support higher ratings.
Comparing current functional limitations with the rating criteria for assigned percentages is important. When symptoms align with higher rating levels but lower percentages were received, ratings may be inadequate.
Bilateral involvement often gets overlooked in initial ratings. When neuropathy affects both feet, ratings for both sides plus the bilateral factor should be received—a 10% increase in combined ratings that can significantly impact compensation. Veterans experiencing this situation should consider requesting a VA disability rating increase to ensure proper recognition of bilateral conditions.
Secondary conditions frequently go unrecognized. Skin problems, balance disorders, or orthopedic issues caused by neuropathy warrant separate ratings that can substantially increase overall disability compensation.
A veteran initially received a 20% rating for neuropathy in his right foot but failed to mention similar symptoms in his left foot during the C&P exam. After documenting bilateral involvement with nerve conduction studies showing abnormalities in both feet, he successfully appealed for separate 20% ratings for each foot, resulting in a combined rating of 36% with the bilateral factor applied.

Documenting Condition Progression
Veterans experiencing worsening symptoms should maintain detailed records of symptom progression, functional decline, and impact on daily activities to support increase claims. This documentation provides the evidence needed to demonstrate that current symptoms warrant higher disability ratings than previously assigned.
Keeping detailed records of how neuropathy has worsened since last ratings is important. Documenting new symptoms, increased pain levels, additional functional limitations, and any new treatments or medications required to manage conditions helps support claims.
Medical records showing progression are important for increase claims. Regular follow-up appointments with documented worsening of symptoms, new diagnostic testing showing progression, or specialist evaluations noting functional decline all support rating increases.
Functional capacity evaluations can provide objective evidence of current limitations compared to previous assessments. These evaluations measure specific abilities like walking distance, standing tolerance, and balance, providing concrete evidence of functional decline.
Appeal Process Options
The VA offers multiple appeal pathways including supplemental claims, higher-level reviews, and Board of Veterans’ Appeals reviews, each with specific timelines and evidence requirements. Understanding these options helps veterans choose the most appropriate path for their situation and maximize their chances of success.
The Appeals Modernization Act created three distinct review options, each designed for different situations. Choosing the right option depends on whether new evidence exists, whether errors were made, or whether fresh reviews of cases are desired.
Supplemental claims work best when new and relevant evidence exists that wasn’t considered in original decisions. This option allows submission of additional medical evidence, updated examinations, or new documentation supporting higher ratings.
Higher-level reviews are appropriate when the VA made errors in reviewing existing evidence. Senior reviewers examine the same evidence with fresh eyes, potentially identifying overlooked information or rating errors. Understanding how to challenge a low VA rating helps veterans navigate these appeal processes effectively.

Advanced Considerations for Neuropathy Claims
Beyond basic rating criteria, veterans must understand complex scenarios including bilateral involvement, secondary conditions, and special monthly compensation that can significantly impact overall disability ratings and compensation. These advanced considerations often make the difference between adequate and optimal disability compensation.
Bilateral Factor and Combined Ratings
When neuropathy affects both feet, veterans may be eligible for bilateral factor calculations that can increase combined disability ratings beyond simple mathematical addition. Understanding these calculations helps veterans ensure they receive full compensation for bilateral conditions and avoid common rating errors.
Bilateral conditions receive special consideration in VA disability calculations because having the same condition in both extremities creates greater functional impairment than simple addition would suggest. The bilateral factor adds 10% to combined ratings when qualifying bilateral conditions exist.
Many veterans don’t realize they qualify for bilateral ratings when neuropathy affects both feet. Even when one side is more severely affected than the other, both sides can receive separate ratings if objective evidence supports bilateral involvement.
The bilateral factor calculation can significantly increase monthly compensation. For example, with 30% ratings for neuropathy in each foot, instead of a 51% combined rating, a 56% combined rating with the bilateral factor applied is received.
Calculating Bilateral Ratings
The VA applies a 10% bilateral factor when the same condition affects corresponding extremities, potentially increasing overall compensation significantly. Understanding this calculation helps veterans ensure they receive proper compensation for bilateral conditions and can identify when ratings may be incomplete.
Bilateral factor calculations follow specific VA mathematics that don’t work like regular addition. The VA first combines bilateral ratings using their standard formula, then adds 10% of that combined rating to determine final percentages.
Each foot must have a separate, ratable condition to qualify for bilateral factor. “Bilateral neuropathy” can’t simply be rated as one condition—individual ratings for left foot neuropathy and right foot neuropathy are needed to qualify for the bilateral factor.
Documentation requirements for bilateral ratings include objective evidence of neuropathy in both feet. This means separate neurological findings, diagnostic testing results, and functional assessments for each side, not just a general statement about bilateral symptoms.
Secondary Condition Ratings
Neuropathy can lead to secondary conditions like falls, skin ulcers, or gait abnormalities that warrant separate disability ratings under different diagnostic codes. These secondary conditions often go unrecognized but can significantly increase overall disability compensation when properly documented and claimed.
Secondary conditions develop as a direct result of service-connected neuropathy and qualify for separate disability ratings. These aren’t just complications—they’re distinct medical conditions caused by primary neuropathy that deserve individual consideration.
Skin conditions represent common secondary issues from neuropathy. Decreased sensation leads to unnoticed injuries, pressure sores, or infections that can be rated separately under dermatological codes. These conditions often require ongoing treatment and can significantly impact quality of life.
Orthopedic problems frequently develop from altered gait patterns caused by neuropathy. When nerve damage changes how walking occurs, it can cause knee, hip, or back problems that warrant separate ratings under musculoskeletal codes.
Special Monthly Compensation (SMC)
Severe cases of neuropathy may qualify for SMC benefits when functional loss reaches specific thresholds, providing additional compensation beyond standard percentage ratings. SMC benefits can substantially increase monthly compensation for veterans with severe functional impairments.
Special Monthly Compensation provides additional benefits beyond regular disability ratings for veterans with severe functional impairments. SMC recognizes that certain levels of disability create extraordinary daily living challenges that warrant additional compensation.
SMC benefits don’t replace regular disability ratings—they’re added on top of percentage-based compensation. This can result in substantial increases in monthly benefits for qualifying veterans with severe neuropathy.
Understanding SMC criteria helps in recognizing when neuropathy might qualify for these enhanced benefits. Many veterans with qualifying conditions never receive SMC simply because they don’t know it exists or don’t understand the criteria.
SMC-K for Loss of Use
Veterans with complete or near-complete loss of use of one or both feet due to severe neuropathy may qualify for SMC-K benefits, adding significant monthly compensation. This benefit recognizes that functional loss equivalent to amputation deserves compensation beyond standard rating percentages.
SMC-K applies when loss of use of a foot is equivalent to anatomical loss (amputation). Severe neuropathy can cause such complete functional impairment that affected feet become essentially useless, qualifying for this enhanced compensation.
Loss of use doesn’t require complete paralysis—it requires functional uselessness. When neuropathy causes such severe weakness, sensory loss, or pain that feet can’t be used for any practical purpose, qualification for SMC-K might exist.
SMC-K for one foot provides substantial additional monthly compensation on top of regular disability ratings. Qualifying for SMC-K for both feet increases compensation even more significantly, recognizing the extraordinary impact of bilateral loss of use.

Specific Action Steps for Veterans
Veterans need a systematic approach to gathering evidence, preparing documentation, and submitting claims to maximize their chances of receiving accurate neuropathy ratings. This section provides concrete, actionable steps that veterans can follow to build strong claims and navigate the VA system effectively.
Step-by-Step Claim Preparation Process
Veterans need a systematic approach to gathering evidence, preparing documentation, and submitting claims to maximize their chances of receiving accurate neuropathy ratings. Following a structured preparation process helps ensure that all necessary evidence is collected and presented effectively to support claims.
Building successful neuropathy claims requires methodical preparation and attention to detail. Random medical appointments and incomplete documentation often result in inadequate ratings that don’t reflect the true severity of conditions.
Starting preparation at least 3-6 months before filing claims is advisable when possible. This timeline allows for gathering comprehensive medical evidence, obtaining necessary testing, and ensuring all documentation meets VA standards before submission.
Creating comprehensive files containing all relevant medical records, service documents, and supporting evidence is important. Organization matters—well-organized claims receive better attention from VA reviewers and reduce the likelihood of important evidence being overlooked.
Medical Evidence Collection Steps
The medical evidence collection process involves five critical steps: obtaining complete service medical records, scheduling comprehensive neurological evaluation, requesting nerve conduction studies and EMG testing, documenting daily symptoms for 30 days, and gathering buddy statements from family and friends about functional limitations.
Step 1: Requesting complete service medical records from the National Personnel Records Center is important. Not relying on what might be in files—ordering everything and reviewing it carefully for any mention of foot problems, injuries, or early symptoms is necessary.
Step 2: Scheduling comprehensive neurological evaluations with qualified specialists is important. Explaining that documentation is needed for VA disability claims and ensuring providers understand the importance of detailed functional assessments and objective findings helps.
Step 3: Obtaining current nerve conduction studies and EMG testing from qualified facilities is necessary. These tests provide objective evidence of nerve damage that the VA reviews and often determine the difference between rating levels.
Step 4: Maintaining detailed symptom diaries for at least 30 days before filing claims is helpful. Documenting daily pain levels, functional limitations, medication effects, and specific examples of how neuropathy impacts activities provides valuable evidence.
Step 5: Collecting buddy statements from family members, friends, or coworkers who can describe how neuropathy affects daily functioning is valuable. These statements provide perspective on functional limitations from people who observe regularly.
A veteran preparing his neuropathy claim documented his symptoms for 45 days, noting that he could only stand for 15 minutes before severe burning pain forced him to sit down, walked with an unsteady gait requiring frequent breaks, and experienced three falls in the past month due to numbness in his feet. This detailed documentation helped support a 40% rating rather than the initial 20% he might have received with less thorough evidence.
Filing Strategy Implementation
Submitting fully developed claims with all evidence included initially, using VA Form 21-526EZ for initial claims, and ensuring all medical evidence is dated within one year of filing reduces processing delays and improves the likelihood of receiving accurate ratings on first decisions.
Submitting fully developed claims (FDC) whenever possible by including all supporting evidence with initial applications is recommended. This approach typically results in faster processing times and more favorable outcomes because the VA can make decisions without requesting additional information.
Using VA Form 21-526EZ for initial disability claims and completing every section thoroughly is important. Incomplete applications create delays and may result in important information being overlooked during the rating process.
Ensuring all medical evidence is current—preferably within the past year of filing—is necessary. Outdated medical records may not accurately reflect current condition severity and can result in lower ratings than symptoms warrant.
Post-Decision Action Steps
After receiving rating decisions, veterans must take specific actions to either accept ratings or pursue additional compensation through appeals or increase requests. Understanding these post-decision options and timelines helps veterans make informed decisions about their next steps.
Rating decision letters contain information about assigned percentages, effective dates, and appeal rights. Reading these documents carefully and not assuming decisions are final when they don’t accurately reflect condition severity is important.
Veterans have one year from decision dates to file appeals without losing their effective dates. However, claims for increased ratings can be filed at any time when conditions worsen or new evidence supporting higher ratings is obtained.
Considering whether assigned ratings accurately reflect functional limitations is important. When significant discrepancies exist between actual symptoms and rating percentages, grounds for appeals or supplemental claims may exist.
Decision Review Timeline
Veterans have one year from the decision date to file appeals, but can file increase claims at any time when conditions worsen or new evidence becomes available. Understanding these timelines helps veterans preserve their rights and choose the most appropriate review option for their situation.
The one-year appeal deadline is important for preserving original effective dates. Filing within this timeframe means any increase in rating will be backdated to original claim dates, potentially resulting in significant retroactive compensation.
Supplemental claims can be filed at any time with new and relevant evidence. These claims establish new effective dates based on when filing occurs, so timing becomes important when gathering additional medical evidence.
Claims for increased ratings don’t have specific deadlines but should be filed promptly when evidence supporting higher ratings exists. Delays in filing can result in lost compensation for periods when higher ratings were qualified for.
Understanding common pitfalls in the VA claims process can help veterans avoid mistakes that lead to denials or inadequate ratings. Veterans should be aware of common VA disability filing mistakes to ensure their neuropathy claims are properly prepared and submitted.
Neuropathy Claim Preparation Checklist:
- ☐ Complete service medical records obtained
- ☐ Current neurological evaluation scheduled
- ☐ Nerve conduction studies/EMG completed within past year
- ☐ 30-day symptom diary completed
- ☐ Buddy statements collected from 3+ observers
- ☐ VA Form 21-526EZ completed thoroughly
- ☐ All medical evidence dated within 12 months
- ☐ Medical opinion linking condition to service obtained
- ☐ Secondary conditions identified and documented
- ☐ Bilateral involvement assessed if applicable
How REE Medical Supports Veterans with Neuropathy Documentation
REE Medical coordinates independent medical evaluations that provide veterans with comprehensive, VA-compliant documentation for neuropathy claims. Through a nationwide network of licensed medical professionals who specialize in disability-focused documentation, REE Medical connects veterans with qualified physicians who understand the specific requirements for neuropathy evaluations.
The coordination process begins with a complimentary consultation to explain how independent medical documentation is developed. REE Medical’s staff coordinates access to licensed healthcare professionals familiar with VA-standardized forms and disability-focused documentation requirements.
Independent evaluations coordinated through REE Medical provide detailed, objective clinical documentation that meets VA formatting standards. These evaluations include comprehensive functional assessments that measure how neuropathy affects daily activities, work capacity, and quality of life.
Veterans can learn more about coordinating VA-compliant medical evaluations by contacting REE Medical for an informational consultation. REE Medical’s team explains the documentation coordination process and connects veterans with independent, licensed medical providers.
Final Thoughts
Getting appropriate VA disability ratings for neuropathy in feet isn’t just about having the condition—it’s about proving its impact through comprehensive medical evidence and understanding the system’s requirements. The difference between a 10% rating and a 60% rating often comes down to documentation quality, not symptom severity.
Neuropathy claim success depends on three critical factors: establishing clear service connection, obtaining thorough medical documentation that meets VA standards, and understanding the specific functional limitations that drive rating percentages. Veterans who approach their claims strategically, with proper preparation and comprehensive evidence, consistently achieve better outcomes than those who rely on basic medical records.
Neuropathy often involves complex considerations like bilateral ratings, secondary conditions, and potential special monthly compensation that can significantly increase overall disability benefits. Inadequate ratings shouldn’t be settled for when additional evidence or proper documentation might support higher compensation levels that better reflect conditions’ true impact on life.
Disclosure
DISCLAIMER: REE Medical, LLC is not a Veterans Service Organization (VSO) or a law firm and is not affiliated with the U.S. Veterans Administration (“VA”). Results are not guaranteed, and REE Medical, LLC makes no promises. REE Medical’s staff does not provide medical advice or legal advice, and REE Medical is not a law firm. Any information discussed, such as, but not limited to, the likely chance of an increase or service connection, estimated benefit amounts, and potential new ratings, is solely based on past client generalizations and not specific to any one patient. The doctor has the right to reject and/or refuse to complete a Veteran’s Disability Benefit Questionnaire if they feel the Veteran is not being truthful. The Veteran’s Administration is the only agency that can make a determination regarding whether or not a Veteran will receive an increase in their service-connected disabilities or make a decision on whether or not a disability will be considered service-connected. This business is not sponsored by, or affiliated with, the United States Department of Veterans Affairs, any State Department of Military and Veterans Affairs, or any other federally chartered veterans service organization.