Understanding VA Disability Ratings: Essential Knowledge for Veterans
The VA disability rating system determines monthly compensation and benefit eligibility for millions of veterans nationwide. This comprehensive guide explains how the rating process works, what types of evidence the VA reviews, and how different claim pathways function within the VA system. Whether approaching an initial claim or considering options after receiving a rating decision, understanding these foundational elements can help veterans make informed decisions about their VA benefits.
Table of Contents
- Understanding the VA Disability Rating Foundation
- How Different Claim Types Function Within the VA System
- Medical Evidence the VA Reviews
- The VA Claims Process
- VA Benefits Beyond Monthly Compensation
- Timing Considerations in the VA System
- When Independent Medical Documentation May Be Helpful
- Key Takeaways
Understanding the VA Disability Rating Foundation
VA disability rating
The VA disability rating system translates the impact of service-connected conditions into standardized percentages ranging from 0% to 100% in 10% increments. These percentages determine monthly compensation amounts and benefit eligibility. According to VA data, understanding how these ratings work helps veterans recognize whether their current rating accurately reflects their condition’s impact on daily functioning and work capacity.
Since 2016, various veteran support programs have assisted over 25,000 disabled veterans, with data revealing that many veterans receive ratings that don’t fully capture the functional limitations caused by their service-connected conditions.
How the Rating System Functions
The VA’s standardized evaluation process relies on the Schedule for Rating Disabilities, which provides specific criteria for evaluating conditions ranging from mental health issues to orthopedic injuries. Each percentage level from 0% to 100% corresponds to measurable differences in how conditions affect daily life and work capacity.
A 0% rating acknowledges service connection but indicates minimal functional impairment. As percentages increase, they reflect progressively greater limitations in work ability and daily activities. The VA assigns these ratings based on the frequency and severity of symptoms documented in medical evidence.
Understanding these rating levels becomes particularly relevant when veterans discover discrepancies between their actual functional limitations and their assigned ratings. Veterans in this situation may explore requesting a VA disability rating increase to ensure compensation accurately reflects their condition’s current impact.
The 10% Increment Structure
Each 10% increment represents specific functional limitations and symptom patterns outlined in VA rating criteria:
- 10%: Minimal functional loss with occasional symptoms
- 30%: More frequent symptoms that interfere with work efficiency
- 70%: Significant impact on ability to maintain employment
- 100%: Total occupational and social impairment
The VA evaluates how diagnoses translate into real-world limitations rather than simply categorizing conditions by name. According to VA Claims Insider data, the average VA rating for PTSD is 70%, making it the #4 most common VA claim with 1,257,940 disabled veterans receiving service-connected compensation for this condition.
Combined Ratings for Multiple Conditions
When veterans have multiple service-connected conditions, the VA applies a specific mathematical formula called the “whole person” theory. The VA does not add percentages together directly.
The VA starts with the highest rating, then applies subsequent ratings to the remaining “whole person” percentage. For example:
| Step | Calculation | Remaining “Whole Person” | Result |
| 1 | Start with highest rating (30% PTSD) | 70% remaining | 30% |
| 2 | Apply 20% knee rating to remaining 70% | 50% remaining | 30% + 14% = 44% |
| 3 | Round to nearest 10% | N/A | 40% Combined Rating |
With a 30% PTSD rating and a 20% knee injury rating, the combined rating calculates to 44%, which rounds to 40%—not 50%.
Bilateral Factor Considerations
Veterans with disabilities affecting paired body parts (both arms, both legs, or paired organs) may receive additional compensation through the bilateral factor. The VA adds 10% of the combined value of bilateral disabilities to the overall rating, recognizing that limitations on both sides create compounded difficulties.
For instance, 20% ratings for both knees result in a 36% combined bilateral rating. The bilateral factor adds 3.6% (10% of 36%), bringing the total to approximately 40% for those knee conditions alone.
How Different Claim Types Function Within the VA System
VA disability rating
The VA processes several distinct types of disability claims, each with unique requirements, timelines, and evidentiary standards. Understanding how these pathways function helps veterans recognize which approach aligns with their specific circumstances.

Initial Claims and Service Connection
Initial claims establish service connection for previously unrated conditions. According to VA regulations, the VA requires three elements for service connection:
- Current Diagnosed Condition: A qualified healthcare provider must diagnose the condition using specific medical terminology and diagnostic codes
- In-Service Incident or Exposure: Evidence of an injury, illness, or exposure during military service
- Medical Nexus: Medical evidence showing it’s “at least as likely as not” that military service caused or aggravated the condition
The in-service element can be documented through service medical records, but the VA also considers buddy statements, unit histories, and sworn testimony when official records are incomplete. Many service members did not report injuries or illnesses during active duty due to mission requirements or career concerns.
The nexus requirement—medical evidence connecting service to current conditions—often presents the most significant challenge in establishing service connection. Veterans beginning this process may benefit from understanding who qualifies for VA disability benefits to determine the most appropriate approach for their circumstances.
Example: A Marine veteran injured his back during a training exercise in 2015 but didn’t seek immediate medical attention due to mission requirements. Three years after discharge, chronic pain led to a diagnosis of degenerative disc disease. The veteran obtained service medical records showing the training incident, post-service medical records documenting the condition, and an independent medical opinion linking the injury to the current diagnosis. The VA ultimately assigned a 40% rating after reviewing this comprehensive evidence.
Increase Claims for Worsening Conditions
When existing service-connected conditions worsen, veterans may file increase claims. The VA compares current condition severity to the previously rated level, requiring clear medical evidence demonstrating sustained worsening that affects daily functioning beyond temporary flare-ups.
Recent hospitalizations, new treatments, increased medication, or documented functional decline support increase claims. The key element is medical records clearly showing progression rather than isolated incidents.
Recent discussions in Congress highlight the importance of accurate disability ratings. According to reports, a GOP senator has proposed a commission to study the VA disability ratings system following concerns about the current evaluation process. This emphasizes the importance of veterans ensuring their claims accurately reflect their conditions’ impact on daily functioning.

Medical Evidence the VA Reviews
Strong medical evidence forms the foundation of VA disability evaluations. However, routine medical care focuses on treatment and symptom management rather than the detailed functional assessments VA raters need for rating determinations.
Why Standard Medical Records May Not Suffice
Regular healthcare providers focus on treating conditions rather than documenting work capacity limitations and functional impacts in the detail VA rating criteria require. VA raters need specific information:
- How often do symptoms occur?
- What triggers symptoms?
- How do symptoms limit work capacity?
- Can the veteran lift, stand, concentrate, or interact effectively with others?
Standard medical notes rarely address these questions comprehensively. This gap explains why many veterans with legitimate, severe conditions receive lower ratings than expected—not because conditions aren’t real or significant, but because medical records don’t translate symptoms into the functional language the VA uses for ratings.
This challenge highlights the importance of medical evidence in VA disability claims, where understanding what documentation the VA requires can significantly impact claim outcomes.

Independent Medical Evaluations
Independent medical evaluations focus specifically on VA rating criteria, assessing conditions through the lens of disability rating schedules. These examinations dedicate time to thoroughly assess functional limitations, and examining physicians structure evaluations to address rating criteria directly.
Unlike routine medical appointments, independent evaluations have no treatment relationship context, which can strengthen credibility with VA raters who seek objective assessments.
Documentation for Service Connection
Establishing service connection requires comprehensive evidence creating a clear timeline from military service to current symptoms:
Service Medical Records: The foundation of service connection, though many conditions weren’t reported during active duty
Buddy Statements: Sworn statements from fellow service members can establish in-service incidents, document symptoms experienced during service, or confirm exposures not officially recorded
Post-Service Medical Records: Treatment sought shortly after discharge strengthens the connection to service-related injuries
According to research, 2,500,581 disabled veterans are service-connected for Tinnitus, making it the #1 most common VA disability claim. This condition is often established through buddy statements and post-service medical evidence since no objective test exists for subjective tinnitus.
The VA Claims Process
The VA claims process involves multiple stages and potential decision points. Understanding these elements allows veterans to recognize how different approaches may affect timelines and outcomes.
Fully Developed Claims
According to VA guidance, Fully Developed Claims (FDC) can reduce processing time to under 90 days when submitted with complete evidence. An FDC includes complete service medical records, current medical evidence, supporting statements, and all relevant documentation.
The FDC process prioritizes claims that provide everything VA raters need upfront. However, if evidence proves incomplete, the FDC benefits may be lost. Veterans considering this approach should understand what evidence the VA reviews for disability claims to ensure comprehensive documentation before submission.
Common Evidence Challenges
“Insufficient medical evidence” is the most common reason for claim delays and denials. The issue typically isn’t that veterans lack medical records, but that records don’t contain the specific functional information VA rating criteria require.
Medical records might clearly show a PTSD diagnosis, but VA raters need documentation of symptom frequency, panic attack occurrence, social isolation, and impacts on work performance and relationships. Without this functional detail, even extensive medical records may be considered insufficient for rating purposes.
Secondary Conditions
Secondary conditions—disabilities caused by primary service-connected conditions—can significantly increase overall ratings but require careful documentation of medical causation establishing clear causal relationships beyond simple correlation.
For example, service-connected back injuries may lead to depression due to chronic pain and limited mobility. The depression could be rated as secondary to the back condition, but medical evidence must establish the causal relationship.
Recent studies highlight this interconnected nature. According to Hill & Ponton, back injuries and spinal conditions are among the most common health issues in veterans, with these conditions often leading to secondary disabilities like depression, anxiety, and mobility issues that can significantly increase combined ratings.
Example: An Army veteran with a 40% rating for service-connected lower back pain developed severe depression and anxiety due to chronic pain limiting activities and social interactions. By obtaining a medical opinion linking mental health conditions to the back disability, the veteran secured additional 70% ratings for depression and anxiety as secondary conditions, bringing the combined rating to 90%.
VA Benefits Beyond Monthly Compensation
VA disability rating
VA disability benefits extend beyond monthly compensation to include special rating considerations, healthcare priorities, and family benefits.
Special Rating Considerations
Certain circumstances allow veterans to receive compensation levels exceeding standard percentage ratings or provide temporary boosts during critical recovery periods.
Individual Unemployability (TDIU)
Individual Unemployability provides 100% disability compensation for veterans who cannot maintain substantially gainful employment due to service-connected disabilities, even when combined ratings don’t reach 100%.
According to VA regulations, TDIU has specific requirements:
| TDIU Type | Requirements | Benefits |
| Schedular TDIU | One condition ≥60% OR combined ≥70% with one condition ≥40% | 100% compensation rate |
| Extraschedular TDIU | Lower ratings but unemployable due to service-connected conditions | 100% compensation rate |
| Temporary TDIU | Temporary unemployability during recovery | 100% rate during qualifying period |
The VA defines substantially gainful employment as work providing income above the federal poverty threshold. Veterans whose disabilities prevent consistent earning at this level may qualify for TDIU regardless of percentage ratings.
Temporary 100% Ratings During Recovery
Per VA guidance, veterans undergoing surgery or extended hospitalization for service-connected conditions may qualify for temporary 100% ratings during recovery periods. These ratings continue until maximum medical improvement is reached and re-evaluation occurs.
For major surgeries, this could mean months of 100% compensation during recovery. The VA must be informed about surgery or hospitalization, as these ratings are not automatic.
Healthcare Access and Priority
VA disability rating levels fundamentally affect healthcare experience within the VA system. Veterans with any service-connected rating receive priority healthcare access over non-service-connected veterans.
At 50% or higher, veterans qualify for comprehensive healthcare coverage for all conditions—not just service-connected ones. This means diabetes, high blood pressure, or any other health issue receives VA healthcare coverage regardless of service connection.
Dependent Benefits
Per VA regulations, veterans rated 30% or higher can claim additional monthly compensation for dependents, including spouses, unmarried children under 18 (or 23 if in school), and dependent parents. Amounts increase with disability ratings.
Dependency and Indemnity Compensation (DIC) provides ongoing support for surviving spouses and children when veterans die from service-connected conditions.
Data shows that 1,474,667 disabled veterans have service-connected knee pain, making limitation of flexion of the knee the #2 most common VA disability claim, with many qualifying for dependent benefits that significantly increase monthly compensation.

Timing Considerations in the VA System
Understanding timing within the VA claims process can affect retroactive compensation amounts and prevent unnecessary delays.
Effective Date Considerations
According to VA regulations, effective dates determine when compensation begins. Several timing rules affect retroactive payments:
Intent to File
Filing an Intent to File form preserves potential effective dates for up to one year while veterans gather evidence. This form costs nothing and takes minutes to complete.
For example, a veteran realizing in January that a PTSD claim should be filed but needing time for medical evaluations could file an Intent to File in January and submit the complete claim in June. If approved, the effective date returns to January—not June.
For a veteran receiving a 70% PTSD rating, that five-month difference could represent over $7,000 in retroactive compensation.
The One-Year Rule for Recent Veterans
Per VA regulations, claims filed within one year of discharge can receive effective dates back to the day after separation, regardless of when filed. After the one-year mark, the effective date becomes the date of claim filing.
Example: A Navy veteran separated in March 2023 but didn’t file for service-connected hearing loss until February 2024—just within the one-year window. When approved at 10%, the effective date returned to the day after separation, resulting in nearly $1,400 in retroactive compensation that would have been lost had filing occurred one month later.
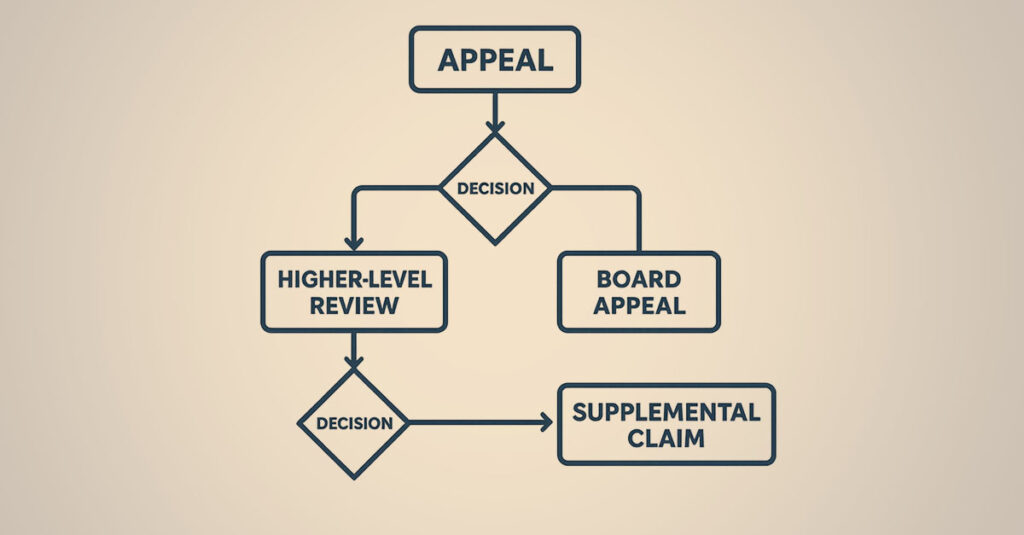
Appeal Options
When initial disability decisions don’t accurately reflect condition severity, the VA offers multiple appeal pathways, each with distinct advantages and timelines. Veterans dealing with unfavorable decisions should understand how to challenge a low VA rating effectively.
Supplemental Claims
According to VA guidance, Supplemental Claims allow submission of new and relevant evidence for reconsideration. This pathway works best when new evidence becomes available—recent medical records, independent medical evaluations, or buddy statements not included originally.
Higher-Level Reviews
Per VA guidance, Higher-Level Reviews involve senior VA raters examining the same evidence with fresh perspective. This option works well when veterans believe evidence clearly supports a higher rating but have no new evidence to submit.
Board Appeals
The Board of Veterans’ Appeals offers three lanes according to VA guidance:
- Direct Review: Fastest option, relies entirely on existing evidence
- Evidence Submission: Allows new evidence but takes longer
- Hearing Request: Allows personal testimony to a Veterans Law Judge

When Independent Medical Documentation May Be Helpful
Professional medical support services can bridge critical gaps by providing specialized evaluations and documentation aligning with VA requirements. This support proves particularly valuable for certain situations:
Situations Where Independent Evaluations May Help
Complex Conditions: Conditions that don’t fit neatly into standard rating categories often benefit from specialized medical opinions. Mental health conditions with multiple symptoms, rare diseases, or conditions with unusual presentations require evaluators understanding both medical complexities and VA rating nuances.
Previous Denials or Low Ratings: When ratings don’t reflect actual symptom severity, independent evaluations can provide missing documentation.
Insufficient Routine Documentation: When regular medical appointments don’t capture the functional limitations VA raters need to see.
Independent Evaluation Benefits
Independent evaluations focus specifically on what the VA reviews: functional limitations, symptom frequency, work capacity impacts, and objective findings supporting claimed disability levels. These evaluations dedicate comprehensive assessment time—something routine medical appointments rarely provide.
The examining physician understands VA rating schedules and structures evaluations to address specific criteria driving rating decisions. The independence factor adds credibility, as these evaluators have no treatment relationship and no financial incentive to provide favorable opinions.
How REE Medical Coordinates Medical Documentation
REE Medical provides veterans with access to independent, licensed medical professionals who deliver detailed medical documentation using VA-standardized forms and DBQs. Our role is to help coordinate documentation so that a veteran’s medical history is clearly organized and presented for potential submission to the VA as part of a claim file.
We’re focused on helping veterans obtain precise, evidence-based documentation that may be submitted as part of the evidence the VA reviews. REE Medical coordinates independent medical evaluations and DBQs prepared by licensed healthcare providers, with the goal of aligning documentation with VA-standardized formats and commonly reviewed medical information. REE Medical does not influence or control how the VA weighs this evidence or what rating it assigns.
REE Medical does not prepare, present, or submit VA disability claims and does not provide legal, medical, or representational services. Our focus is on coordinating high-quality, objective medical evaluations and documentation with independent, licensed healthcare professionals.
For veterans who feel their medical evidence is limited, who have experienced previous claim challenges, or whose conditions are not fully documented in existing records, REE Medical offers access to detailed independent medical evaluations and DBQs that may be submitted to the VA as part of a disability claim. Our nationwide network of independent providers allows veterans in many areas to schedule evaluations, and transparent pricing is intended to reduce uncertainty and support objectivity. The VA alone determines whether any documentation results in a change to disability ratings or benefits.
Whether pursuing an initial claim for a diagnosed but unrated condition or seeking an increase for a worsened service-connected disability, REE Medical coordinates medical documentation support that helps veterans organize and present additional clinical information to the VA as part of their evidence. REE Medical does not guarantee outcomes and does not advise on how to file, present, or argue VA disability claims.
Contact REE Medical for an informational consultation about coordinating independent medical documentation. These consultations are educational in nature and are not a substitute for legal advice, medical care, or assistance from an accredited representative.
Key Takeaways
The VA disability rating system involves multiple interconnected elements that affect compensation and benefits:
- VA disability ratings range from 0% to 100% in 10% increments, directly impacting monthly compensation and benefit access
- The VA uses a “whole person” formula for multiple conditions—percentages are not simply added together
- Strong medical evidence focusing on functional limitations forms the cornerstone of VA rating evaluations
- Fully Developed Claims can reduce processing time to under 90 days when submitted with complete evidence
- Individual Unemployability (TDIU) can provide 100% compensation even with lower combined ratings
- Filing an Intent to File preserves effective dates for up to one year while gathering evidence
- Independent medical evaluations can bridge critical documentation gaps for complex conditions
Understanding the VA disability rating system helps veterans recognize whether current ratings accurately reflect their conditions’ impacts. The system evaluates how service-connected conditions affect daily functioning and work capacity, translating these impacts into percentage ratings that determine compensation and benefit eligibility.
Armed with knowledge about how the VA evaluates claims, what evidence the VA reviews, and how different pathways function, veterans can make informed decisions about their disability benefits. Initial claims and increase claims help veterans obtain the disability benefits they earned through service.
DISCLAIMER: REE Medical, LLC is not a Veterans Service Organization (VSO) or a law firm and is not affiliated with the U.S. Veterans Administration (“VA”). Results are not guaranteed, and REE Medical, LLC makes no promises. REE Medical’s staff does not provide medical advice or legal advice, and REE Medical is not a law firm. Any information discussed, such as, but not limited to, the likely chance of an increase or service connection, estimated benefit amounts, and potential new ratings, is solely based on past client generalizations and not specific to any one patient. The doctor has the right to reject and/or refuse to complete a Veteran’s Disability Benefit Questionnaire if they feel the Veteran is not being truthful. The Veteran’s Administration is the only agency that can make a determination regarding whether or not a Veteran will receive an increase in their service-connected disabilities or make a decision on whether or not a disability will be considered service-connected. This business is not sponsored by, or affiliated with, the United States Department of Veterans Affairs, any State Department of Military and Veterans Affairs, or any other federally chartered veterans service organization.