If you’re a veteran dealing with poor sleep, loud snoring, or daytime exhaustion, you’re not alone—and your VA rating for sleep apnea can make a real difference in your benefits and quality of life.
We’ll walk you through exactly what the VA looks for: how ratings are decided, what evidence strengthens your claim, and how upcoming changes could affect your benefits. By the end, you’ll know how to approach your claim with confidence REE Medical connects veterans with independent, licensed medical professionals who provide thorough and accurate documentation to support their VA disability claim.
This guide explains the types of service connection recognized by VA (direct, secondary, or toxic-exposure related), what veterans can generally expect during a C&P exam, and what options may exist if a veteran disagrees with a VA rating decision.
TL;DR: Your Key Takeaways
- Sleep Apnea is Common: Many veterans have sleep apnea, and getting the right VA rating is crucial for benefits.
- How Ratings Work: The VA rates sleep apnea from 0% to 100% based on how bad it is, what treatment you need, and if it causes other problems.
- Getting Service Connection: VA requires evidence that sleep apnea is connected to military service. This may be through direct service evidence, as a secondary condition, or, in limited cases, under presumptive rules.
- Evidence is Key: A sleep study and a completed Disability Benefits Questionnaire (DBQ) are often critical evidence VA considers when deciding a claim.
- CPAP Use Matters: Using a CPAP machine usually gets you a 50% rating now, but this might change.
- Proposed Changes: The VA might change how they rate sleep apnea soon, focusing more on symptoms than just CPAP use.
- How to Increase Your Rating: The VA may increase a veteran’s rating if new evidence shows the condition has become more severe or has greater impact on daily life. Updated sleep studies, medical evaluations, and treatment records can provide information the VA uses when reviewing a rating.
REE Medical REE Medical can help by connecting you with qualified providers who are experienced in completing Disability Benefits Questionnaires (DBQs). These evaluations provide detailed medical information that VA may use when reviewing a claim.
What Is Sleep Apnea and How Does the VA Rate It?
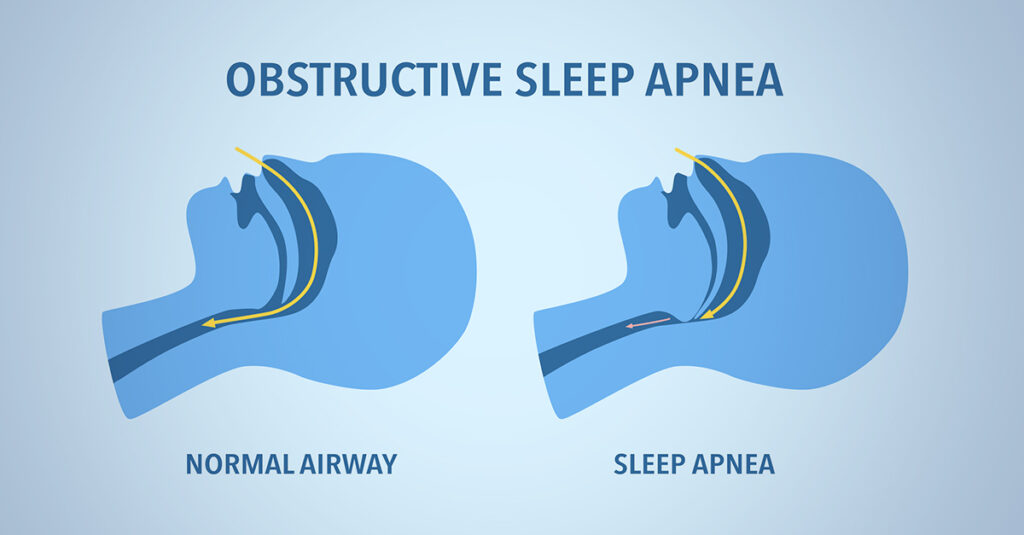
Sleep apnea is a serious sleep disorder where breathing repeatedly stops and starts during the night. This can happen because:
- Obstructive Sleep Apnea (OSA): the airway becomes physically blocked, often due to relaxed throat muscles.
- Central Sleep Apnea (CSA): the brain fails to send proper signals to the breathing muscles.
- Mixed/Complex Sleep Apnea: a combination of both obstructive and central causes.
These interruptions in breathing can occur dozens or even hundreds of times per night. Common symptoms include loud snoring, choking or gasping during sleep, morning headaches, and excessive daytime fatigue. Over time, untreated sleep apnea increases the risk of high blood pressure, heart disease, stroke, diabetes, and cognitive decline (NIH – Sleep Apnea).
The gold standard treatment is the use of a Continuous Positive Airway Pressure (CPAP) machine, which keeps the airway open by delivering steady air pressure through a mask. Other treatment options include oral appliances, lifestyle changes, surgery, and—in some cases—implanted devices (American Academy of Sleep Medicine). Accurate diagnosis usually requires a sleep study (polysomnography).
What Are the Different Types of Sleep Apnea?
There are three main types of sleep apnea:
- Obstructive Sleep Apnea (OSA): This is the most common type. It happens when the muscles in your throat relax too much and block your airway while you sleep. You might snore loudly and your oxygen levels can drop.
- Central Sleep Apnea (CSA): This type is less common. It occurs when your brain doesn’t send the proper signals to the muscles that control breathing. You stop breathing, but not because of a blockage.
- Mixed Sleep Apnea: This is a combination of both obstructive and central sleep apnea. You experience both airway blockages and pauses in breathing due to brain signals.
Each type needs to be diagnosed carefully. The VA looks at things like your apnea index (how many times you stop breathing per hour) and how low your oxygen levels get when deciding your rating. Knowing the type you have helps your medical provider document your condition accurately.
How Does the VA Disability Rating Schedule Work for Sleep Apnea?
Before filing a VA claim, it’s important to understand how the VA evaluates sleep apnea. Ratings fall under Diagnostic Code 6847 of the VA Schedule for Rating Disabilities. The rating is based on the severity of symptoms and the type of treatment required.
| Rating Percentage | What It Means | Treatment Needed |
| 0 percent | You have a sleep disorder diagnosis but are asymptomatic, or symptoms don’t interfere with daily functioning. | No device or special treatment is required. |
| 30 percent | You experience persistent daytime hypersomnolence (excessive daytime sleepiness). | May use dental/oral appliance or lifestyle modifications, but not necessarily a CPAP. |
| 50 percent | Your condition requires the use of a breathing assistance device such as a CPAP machine. | Nightly CPAP (Continuous Positive Airway Pressure) or other breathing assistance. |
| 100 percent | You have chronic respiratory failure with carbon dioxide retention, develop cor pulmonale (right-sided heart failure), or require a tracheostomy. | Advanced respiratory support, oxygen therapy, or surgical airway intervention. |
This table shows how your symptoms, any related health issues, and whether you need a breathing device can lead to a specific rating. Knowing where you fit helps you gather the right proof, like sleep study results or records of your CPAP use.
VA evaluates sleep apnea under its Schedule for Rating Disabilities, found in 38 C.F.R. § 4.97, Diagnostic Code 6847. This regulation explains the criteria VA uses when assigning percentages for sleep apnea.
What Are the Proposed VA Rating Changes for Sleep Apnea in 2025?
The VA is considering changes to how sleep apnea is rated under Diagnostic Code 6847, but nothing is final yet. Below are proposals and what veterans should watch out for:
- CPAP use may no longer automatically qualify for a veteran for a 50% rating. Instead, treatment effectiveness will likely matter more.
- A new 10% rating tier might be introduced for cases where symptoms are only partially relieved, or the veteran cannot tolerate a device like CPAP.
- There are reports that the 30% rating could be eliminated, so future sleep apnea ratings might be limited to 0%, 10%, 50%, and 100%.
- Greater use of objective measures like sleep study results (for example, oxygen levels, apnea-hypopnea index) may play a bigger role in determining ratings. Also, veterans’ ability to tolerate devices, or whether CPAP is effective for them, may factor in.
- Existing ratings or claims filed before any changes to take effect may be “grandfathered” under the old rules, meaning those veterans maintain their current rating unless they request a review.
How Can Veterans Establish Service Connection for Sleep Apnea?
To get VA benefits for sleep apnea, you need to prove it’s connected to your time in the military. This is called “Service Connection.” There are three main ways to do this: direct, secondary, or presumptive. Understanding these is the first step to building a strong claim.
What Is Direct Service Connection, and How Do You Prove It?
Direct service connection means you need to show that your sleep apnea started or got worse while you were in the military. To do this, you’ll need:
- Military Medical Records: Show that you have complained about sleep problems or breathing issues during your service.
- Current Diagnosis: Proof from a doctor that you currently have sleep apnea, usually confirmed by a sleep study.
- Buddy Statements: Letters from fellow service members or family who can say they noticed your sleep problems when you were in the service.
Can Sleep Apnea Be a Secondary Condition for VA Disability?
Yes, sleep apnea can often be claimed as a secondary condition. This means it’s caused or made worse by another condition you already have that’s connected to your service. Some common examples include:
- PTSD: The stress and sleep disturbances from PTSD can lead to or worsen sleep apnea.
- Rhinitis or Sinusitis: Chronic nasal problems can block your airway and contribute to sleep apnea.
- Hypertension or Obesity: These conditions, sometimes linked to service stress or lifestyle, can put extra strain on your breathing during sleep.
To prove a secondary connection, you need a medical opinion stating that it’s “at least as likely as not” that your service-connected condition caused or worsened your sleep apnea.
Is Sleep Apnea a Presumptive Condition for VA Benefits?
Currently, sleep apnea is not automatically considered a “presumptive” condition just because you served.
However, if you were exposed to airborne hazards or toxic substances (from burn pits or dust storms) during your service, you might be able to claim it under newer rules for toxic exposures.
If you have sleep apnea and served in certain areas or during specific times where toxic exposures were known, documenting this exposure along with your diagnosis can strengthen your claim.
What Evidence Is Required for a Successful Sleep Apnea VA Claim?

To win your sleep apnea claim, you need strong evidence. This means having objective medical proof, detailed questionnaires, and professional opinions. Putting all this together creates a solid case that meets the VA’s requirements.
Why Is a Sleep Study Critical for Your VA Claim?
A sleep study, also called a polysomnogram, is essential. It objectively measures things like your apnea-hypopnea index (AHI) and how low your oxygen levels drop. These numbers show how severe your sleep apnea is.
- Without a sleep study, the VA can’t see the key numbers that define your condition’s severity.
- Your doctor or the VA examiner won’t have the data needed to assign an accurate rating.
- You might get a lower rating because there isn’t enough detailed information about your breathing problems during sleep.
A complete sleep study report is the foundation of your claim. It helps with service connection and determining your rating.
How to Complete and Use the Sleep Apnea Disability Benefits Questionnaire (DBQ)?
The Sleep Apnea DBQ is a form that doctors use to report on your diagnosis, symptoms, and how sleep apnea affects you. To make it as effective as possible:
- Get the latest version of the DBQ from VA.gov or your VA medical center.
- Have a qualified sleep specialist fill out the form completely. Make sure they cover daytime sleepiness, device use, and any lung function results.
- Double-check that the form is filled out accurately and includes all necessary lab results and treatment records. Missing information can cause delays or denials.
A well-filled-out DBQ makes it easier for the VA to understand your condition and apply the correct rating criteria.
What Is a Nexus Letter and How Does It Strengthen Your Claim?
A nexus letter is a medical opinion from a doctor that clearly links your sleep apnea to your military service or another service-connected condition. A strong nexus letter should:
- State clearly that your condition is “at least as likely as not” related to your service. This is the standard the VA uses.
- Summarize your military and medical history in a way that shows the connection.
- Explain the medical reasons why your service caused or worsened your sleep apnea.
This letter turns medical facts into a strong argument for your claim, reducing the chance of denial due to a weak link to service.
What Does the VA Evaluate for Sleep Apnea?

When reviewing a sleep apnea claim, the VA refers to Diagnostic Code 6847, which outlines how different levels of severity are rated. This diagnostic code focuses on factors such as:
- Documented diagnosis of sleep apnea confirmed by a sleep study.
- Treatment details, including whether a CPAP or other breathing device is required.
- Symptoms and daily impact, such as excessive daytime sleepiness or fatigue.
These details help the VA determine the appropriate disability rating based on how significantly the condition affects your daily life and overall health.
How Independent Providers Document Sleep Apnea
REE Medical connects veterans with independent, licensed medical professionals who provide thorough Disability Benefits Questionnaires (DBQs) and medical evaluations. These DBQs capture the same objective information the VA considers when making rating decisions — including sleep study data, treatment adherence, and the presence of ongoing symptoms.
The goal of these independent evaluations is to ensure your condition is clearly and accurately documented before you decide whether to submit evidence to the VA.
Why This Matters
Accurate, detailed medical documentation from independent providers helps the VA make a well-informed decision on your claim. While REE Medical does not prepare or submit claims, the company ensures veterans have access to competent, transparent medical evidence that aligns with VA evaluation standards.
How Can Veterans Navigate the VA Claims and Appeals Process for Sleep Apnea?

Filing a VA claim can seem complicated, but knowing the steps can make it easier. If your VA disability claim is denied, there are ways to appeal and still get the benefits you’ve earned.
What Are the Steps to File a VA Claim for Sleep Apnea?
To start your claim:
- VA Form 21-526EZ, which is the standard form used when a veteran applies for disability compensation.
- Medical evidence, such as a completed sleep study that confirms a diagnosis of sleep apnea.
- Supporting documentation, including a Disability Benefits Questionnaire (DBQ) from a qualified medical provider that outlines current symptoms, treatment methods, and severity.
These materials help the VA determine whether a condition is service-connected, and what rating level may apply under Diagnostic Code 6847.
What Are Common Reasons for Sleep Apnea Claim Denials?
Many sleep apnea claims are denied for a few common reasons:
- Lack of Service Evidence: Not enough proof showing the condition started or worsened during service. This could be missing medical records from your service time or no buddy statements.
- Incomplete Medical Data: Missing information from your sleep study or other medical tests. The VA needs complete data to make a decision.
Knowing these common pitfalls can help you gather the right evidence to avoid them or strengthen your case if you need to appeal.
How Do You Appeal a Denied Sleep Apnea VA Claim?
When a VA disability claim is denied, veterans have several appeal options available through the Department of Veterans Affairs. Each pathway allows the VA to review the claim in a different way:
- Supplemental Claim: This review option allows the VA to consider new and relevant evidence that was not part of the original claim record.
- Higher-Level Review: A senior VA reviewer re-examines the claim using the evidence already on file to determine if a different outcome is warranted.
- Board of Veterans’ Appeals (BVA): Veterans may choose to have their case reviewed by the BVA, which conducts a more formal review process and may hold hearings as part of its evaluation.
Each appeal lane has specific requirements for what types of evidence can be considered. Independent medical documentation—such as updated DBQs or medical opinions—can help ensure the veteran’s health information is complete and accurately represented before submission to the VA.
What the VA Considers When Reviewing an Increased Rating for Sleep Apnea
When a veteran requests an increased disability rating, the VA evaluates whether new medical evidence demonstrates that the condition has become more severe. For sleep apnea, the VA typically reviews:
- Recent Sleep Studies: Updated medical testing, such as a sleep study that measures the apnea-hypopnea index (AHI), may provide information about whether the condition has worsened over time.
- Related Health Complications: The VA also considers whether sleep apnea has contributed to other serious health issues—such as chronic respiratory failure or cor pulmonale (heart complications)—which can affect the overall rating level.
Independent medical professionals coordinated through REE Medical can document these changes through thorough and objective DBQs, ensuring that the medical evidence clearly reflects the veteran’s current condition.
How Does Using a CPAP Machine Affect Your VA Disability Rating?

Using a CPAP machine is the main treatment for sleep apnea, and it plays a big role in how the VA rates your condition. Understanding the role of prescribed treatments helps explain how the VA determines rating levels for sleep apnea cases.
Why Does CPAP Use Typically Qualify for a 50% VA Rating?
According to the VA Schedule for Rating Disabilities (38 C.F.R. § 4.97, Diagnostic Code 6847), veterans diagnosed with sleep apnea who require the use of a CPAP or similar breathing assistance device may qualify for a 50% disability evaluation.
This rating level reflects the VA’s recognition that ongoing medical treatment is needed to manage a chronic breathing condition that significantly affects daily functioning. Documentation from a licensed medical professional—such as a completed Disability Benefits Questionnaire (DBQ) or medical record confirming CPAP prescription and use—provides objective information for the VA reviews when determining severity.
What Are the Implications of Proposed VA Changes on CPAP Ratings?
The Department of Veterans Affairs has proposed updates to the Schedule for Rating Disabilities that could change how sleep apnea is evaluated beginning in 2025. Under the proposed criteria, ratings would place greater emphasis on the severity of symptoms and functional limitations, rather than the automatic use of a CPAP or other breathing assistance device.
If implemented, the new standards would focus on measurable factors such as:
- The frequency and severity of symptoms like daytime fatigue or cognitive impairment,
- Objective clinical findings from sleep studies, including oxygen desaturation levels, and
- The impact of the condition on daily functioning and overall health.
These proposed updates are not yet finalized. Veterans can review official rulemaking updates in the Federal Register or on VA.gov to stay informed about any changes once they take effect.
How the VA reviews CPAP compliance information
When evaluating sleep apnea under Diagnostic Code 6847, the Department of Veterans Affairs may review documentation showing that a veteran’s condition requires the use of a CPAP or other breathing-assistance device.
Typical sources of medical information can include:
- Device usage data recorded by CPAP equipment,
- Sleep-study results and clinical progress notes from a treating provider, and
- Physician documentation confirming ongoing treatment needs.
These materials help the VA understand the severity and management of sleep-related breathing disorders.
REE Medical coordinates independent, licensed medical professionals who provide objective DBQs and clinical documentation reflecting current treatment and symptom severity. REE Medical does not prepare, present, or submit VA disability claims.
What Resources and Support Are Available for Veterans with Sleep Apnea?

Veterans managing sleep apnea have access to several federal, community, and health-based programs that support long-term care and well-being.
- The Department of Veterans Affairs (VA) offers medical treatment options, including sleep studies and CPAP therapy, through its healthcare system.
- VA Whole Health programs and telehealth services can help veterans integrate sleep hygiene, stress management, and lifestyle strategies into their care.
- Nonprofit organizations such as the American Sleep Apnea Association (ASAA) and the National Sleep Foundation (NSF) provide education, peer support, and public health resources for individuals with sleep-related breathing disorders.
Where Can Veterans Find Local and National Support for Sleep Apnea?
Veterans have access to a range of medical and community-based resources for the diagnosis and management of sleep apnea:
- VA Sleep Centers: Many Department of Veterans Affairs medical centers include sleep clinics that provide evaluation, testing, and treatment for sleep-related breathing disorders.
- Accredited Veterans Service Organizations (VSOs): Organizations such as the Disabled American Veterans (DAV), Veterans of Foreign Wars (VFW), and The American Legion are recognized by VA to assist veterans with benefits inquiries and representation before the VA.
- Peer and Educational Support Networks: Groups like the American Sleep Apnea Association (ASAA) and local community health organizations host support forums, awareness events, and educational materials to help individuals better understand and manage sleep apnea.
These resources focus on medical care, education, and accredited representation, giving veterans access to reliable information and qualified assistance.
How Does REE Medical Support Veterans with Sleep Apnea Documentation?
REE Medical connects veterans with independent, licensed medical professionals who provide thorough and objective Disability Benefits Questionnaires (DBQs) and supporting medical documentation related to sleep apnea.
These independent evaluations capture key clinical details — such as sleep study results, treatment device use, and symptom severity — in the structured format the VA uses for its disability rating process.
By coordinating high-quality, neutral medical evidence, REE Medical ensures veterans have clear and accurate documentation to include in their records when working with accredited representatives or filing independently through VA channels.
REE Medical’s role is strictly medical coordination, not claim preparation or representation. The company does not prepare, present, or submit VA disability claims but provides veterans with transparent access to competent medical documentation that supports fair and timely decision-making by the VA.
Schedule a Free Consultation Today
Whether you’re filing a new claim or appealing a denial, let expert coordination help strengthen your Sleep Apnea VA disability case.
Sleep apnea can significantly impact your life and your ability to work. By understanding how the VA rates it, how to prove service connection, and what evidence is needed, you can improve your chances of getting the benefits you deserve. Don’t go through this complex process alone. Getting expert help can make a huge difference in your VA disability journey.
Frequently Asked Questions
What lifestyle changes can help manage Sleep Apnea symptoms?
According to the U.S. Department of Veterans Affairs (VA) and the National Heart, Lung, and Blood Institute (NHLBI), certain lifestyle factors can affect the severity of sleep apnea. Maintaining a healthy weight and limiting alcohol or sedative use before bedtime can reduce airway obstruction. Regular physical activity and consistent sleep schedules also contribute to better sleep quality. These adjustments are part of the broader clinical guidance many providers follow when managing sleep-related breathing disorders.
Are there alternative treatments for Sleep Apnea besides CPAP?
The VA and the American Academy of Sleep Medicine (AASM) note that treatment for sleep apnea depends on its type and severity. Continuous Positive Airway Pressure (CPAP) remains the standard therapy, but alternatives exist. Oral appliances, which reposition the jaw or tongue, may be used for mild to moderate cases. In some situations, surgery may be recommended to address structural airway issues. Veterans should consult a licensed sleep specialist to determine which evidence-based treatment aligns with their diagnosis.
How does Sleep Apnea affect mental health in veterans?
Research from the VA’s National Center for PTSD shows a strong connection between sleep apnea and mental health conditions such as depression, anxiety, and posttraumatic stress disorder (PTSD). Disrupted sleep can heighten mood changes, irritability, and concentration difficulties. Effective treatment of sleep apnea—under the guidance of a medical professional—can improve overall well-being and may lessen the severity of co-occurring symptoms.
What role does a sleep study play in diagnosing Sleep Apnea?
A sleep study (polysomnography) is the diagnostic standard recognized by the VA and Department of Defense Clinical Practice Guidelines. During the study, medical professionals monitor breathing patterns, oxygen levels, and brain activity to determine the presence and severity of sleep apnea. This objective data helps clinicians confirm a diagnosis and recommend appropriate medical treatment options.
Can Sleep Apnea lead to other health complications?
Yes. The Centers for Disease Control and Prevention (CDC) and VA Health Library report that untreated sleep apnea can increase the risk of high blood pressure, heart disease, stroke, and type 2 diabetes. Ongoing fatigue from poor sleep can also affect daily functioning and safety. Early diagnosis and consistent treatment are important to minimize these health risks.
How does the VA handle denied sleep apnea claims?
If your sleep apnea claim is denied, it’s important to understand why and take the right steps. You can file a Supplemental Claim if you have new and important evidence that wasn’t considered before. You can also request a Higher-Level Review, where a senior VA reviewer will look at your claim again based on the existing evidence. If those options don’t work, you can appeal to the Board of Veterans’ Appeals (BVA) for a formal hearing. Getting help from a Veterans Service Officer can also be very useful throughout the appeals process.
Conclusion
Understanding how the VA rates sleep apnea is vital for veterans seeking the benefits they’ve earned. By learning about the rating criteria, how to connect your condition to service, and what evidence you need, you can significantly boost your chances of a successful claim. Don’t try to navigate this complex process alone. Consider reaching out for expert support to guide you every step of the way. Taking action now and exploring how specialized assistance can empower your VA disability journey is key.
Ready to strengthen your Sleep Apnea VA disability case? Schedule a Free Consultation Today
Disclosure
DISCLAIMER: REE Medical, LLC is not a Veterans Service Organization (VSO) or a law firm and is not affiliated with the U.S. Veterans Administration (“VA”). Results are not guaranteed, and REE Medical, LLC makes no promises. REE Medical’s staff does not provide medical advice or legal advice, and REE Medical is not a law firm. Any information discussed, such as, but not limited to, the likely chance of an increase or service connection, estimated benefit amounts, and potential new ratings, is solely based on past client generalizations and not specific to any one patient. The doctor has the right to reject and/or refuse to complete a Veteran’s Disability Benefit Questionnaire if they feel the Veteran is not being truthful. The Veteran’s Administration is the only agency that can make a determination regarding whether or not a Veteran will receive an increase in their service-connected disabilities or make a decision on whether or not a disability will be considered service-connected. This business is not sponsored by, or affiliated with, the United States Department of Veterans Affairs, any State Department of Military and Veterans Affairs, or any other federally chartered veterans service organization.