VA Rating for Plantar Fasciitis: Understanding the Evaluation Process and What Veterans Need to Know
Plantar fasciitis affects countless veterans, with recent studies identifying particularly high rates among Army and Marines service members, especially black and female veterans. Understanding how the VA evaluates and rates this condition provides valuable insight into the disability compensation process and monthly benefit amounts that may be available based on documented symptom severity and functional limitations.
Table of Contents
- Understanding VA Disability Ratings for Plantar Fasciitis
- Bilateral Plantar Fasciitis Considerations
- Claim Filing Strategies and Processes
- Medical Documentation and Evidence Standards
TL;DR
- VA ratings for plantar fasciitis range from 10% to 40% based on symptom severity, functional limitations, and treatment response
- Bilateral plantar fasciitis qualifies for additional compensation through the bilateral factor calculation
- Strong medical documentation and proper DBQ completion are central to accurate ratings
- Service connection requires clear evidence linking military service to plantar fasciitis development through direct injury, repetitive stress, or aggravation of pre-existing conditions
- Independent medical evaluations can provide comprehensive evidence to support the VA’s review process
- Common issues include insufficient medical evidence, inadequate symptom reporting, and service connection documentation gaps

Understanding VA Disability Ratings for Plantar Fasciitis
The VA evaluates plantar fasciitis using specific diagnostic codes within their Schedule for Rating Disabilities, with compensation ranging from 10% to 40% depending on how severely the condition impacts daily functioning. The rating process examines pain levels, mobility restrictions, and response to treatment, with each percentage point directly translating to monthly compensation amounts.
The VA’s evaluation focuses on measurable factors rather than subjective reports. Medical documentation showing objective evidence of plantar fasciitis severity carries significant weight in the rating determination process.
Decoding the VA’s Rating Scale and Diagnostic Criteria
The VA uses established diagnostic codes that focus on measurable factors like pain intensity, mobility restrictions, and treatment effectiveness. These ratings follow specific criteria that determine monthly compensation amounts and require particular types of medical documentation.
The rating system breaks down into four main categories:
A 10% rating covers mild symptoms with minimal interference in daily routines. Veterans can typically walk, work, and function normally most days, though some discomfort may occur.
A 20% rating reflects moderate symptoms beginning to affect daily activities. Veterans may experience limping in the mornings or avoid certain physical tasks because of pain.
At 30%, severe symptoms significantly limit activity levels. Walking distance might be restricted, and modifications to work and recreational activities are often necessary.
The highest rating of 40% applies to cases where plantar fasciitis causes marked functional impairment. Veterans may require assistive devices like orthotics or canes, and ability to perform basic activities is seriously compromised.
Breaking Down Standard Rating Percentages
Each rating percentage corresponds to specific symptom severity levels and functional limitations. Understanding these distinctions helps clarify where different conditions might fall within the rating schedule.
| Rating | Severity Level | Functional Impact | Treatment Response |
| 10% | Mild symptoms | Minimal daily interference | Responds well to prescribed treatment |
| 20% | Moderate symptoms affecting one foot | Daily activities impacted | No relief from non-surgical/surgical treatment |
| 30% | Severe symptoms affecting both feet | Significant activity limitations | No relief from non-surgical/surgical treatment |
| 40% | Loss of use | Marked functional impairment | Complete loss of foot function |
At the 10% level, mild heel pain doesn’t significantly impact daily activities. Morning stiffness may occur but resolves quickly and doesn’t interfere with work or exercise.
The 20% rating reflects moderate symptoms affecting daily activities. Pain persists longer, certain movements may be avoided, and walking patterns could be slightly altered.
At 30%, severe symptoms create significant limitations. Walking distances are restricted, persistent pain occurs throughout the day, and work duties or recreational activities have likely been modified.
The 40% rating addresses the most severe cases requiring assistive devices or causing marked functional impairment. Custom orthotics may be necessary, constant pain may occur, or difficulty performing basic job functions may be present.
Documentation Requirements at Each Rating Level
Higher ratings demand more comprehensive medical evidence demonstrating disability and functional limitations. The VA requires specific types of documentation including range of motion measurements, pain assessments, and treatment history records to justify each rating level.
For any rating, basic medical records showing plantar fasciitis diagnosis and treatment history are necessary. Higher ratings require substantially more detailed evidence.
Range of motion measurements become important for ratings above 10%. Medical documentation needs to record exactly how plantar fasciitis limits ankle flexibility and foot movement.
Pain scale assessments should be consistent and well-documented. The VA reviews objective measures of pain levels through standardized assessment tools.
Functional capacity evaluations carry significant weight, especially for 30% and 40% ratings. These tests measure specific capabilities and limitations related to plantar fasciitis.
Treatment history documentation shows the VA how the condition has been managed over time. Failed conservative treatments often support higher ratings because they demonstrate symptom severity and persistence despite treatment attempts.
Consider Marine veteran Sarah M., who initially received a 10% rating for plantar fasciitis. Her medical records showed morning heel pain that improved with activity. After documenting failed physical therapy, steroid injections, and persistent pain affecting both feet during her 12-hour nursing shifts, the VA ultimately assigned a 30% rating. The comprehensive documentation showing bilateral involvement and failed treatments despite her continued work efforts was part of the evidence the VA reviewed.
How Ratings Translate to Monthly Compensation
VA disability ratings directly determine monthly compensation amounts, with 2025 rates ranging from approximately $171 for a 10% rating to over $750 for a 40% rating. These amounts can increase significantly when combined with other service-connected conditions through the VA’s combined rating formula.
Monthly compensation depends on the total combined rating from all service-connected conditions. For plantar fasciitis alone:
- 10% rating: Around $171 monthly
- 20% rating: Approximately $342 monthly
- 30% rating: About $524 monthly
- 40% rating: Over $750 monthly
When veterans have other service-connected conditions, the VA uses a combined rating formula that could result in total ratings higher than simple addition would suggest. Understanding 2025 VA disability compensation rates allows veterans to calculate potential benefits from plantar fasciitis ratings.
Medical Evidence Standards and DBQ Requirements
Strong medical documentation forms the foundation of accurate plantar fasciitis ratings, with Disability Benefits Questionnaires serving as the primary evaluation tool. The VA requires specific clinical findings, diagnostic test results, and functional assessments to determine appropriate ratings.
The VA relies heavily on Disability Benefits Questionnaires (DBQs) to evaluate plantar fasciitis claims. These comprehensive medical evaluations must be completed by qualified healthcare providers who understand VA rating criteria.
Medical evidence needs to present a complete picture of how plantar fasciitis affects daily life. Vague reports about foot pain provide limited value. The VA reviews objective, measurable data that supports claimed disability levels.
Essential Clinical Documentation Requirements
Comprehensive medical records must include detailed physical examination findings, imaging results, gait analysis, and objective measurements that demonstrate the condition’s impact on daily functioning. This documentation provides the foundation for accurate disability rating determinations.
Like other conditions requiring detailed medical evidence, plantar fasciitis claims benefit from thorough documentation. Understanding what evidence supports disability claims helps clarify comprehensive documentation needs.
Medical records should include detailed physical examination findings that extend beyond general pain reports. The VA reviews specific measurements, test results, and objective observations.
Imaging results from X-rays, MRI, or ultrasound can provide evidence of plantar fasciitis severity. These tests might show heel spurs, tissue thickening, or other structural changes that support disability claims.
Gait analysis documentation shows how plantar fasciitis affects walking patterns. Changes in gait can indicate significant functional limitations that support higher ratings.
Objective measurements of heel pain, morning stiffness duration, and activity limitations provide quantifiable evidence of the condition’s impact. The more specific and measurable the documented symptoms, the clearer the medical record becomes.
DBQ Completion Best Practices
Disability Benefits Questionnaires must be completed by qualified medical professionals who understand VA rating criteria and can provide detailed documentation of symptom frequency, intensity, duration, and functional impact on work and daily activities.
The quality of DBQ completion significantly impacts claim outcomes. Not all healthcare providers understand VA rating criteria, so selecting qualified medical professionals matters.
Examining physicians need to document symptom frequency—how often plantar fasciitis pain and limitations occur. Daily symptoms carry more weight than occasional discomfort.
Intensity measurements should be specific and consistent. Using standardized pain scales and functional assessment tools provides objective data the VA can evaluate.
Duration documentation shows how long symptoms persist and how they’ve progressed over time. Chronic, worsening symptoms typically support higher ratings than acute, improving conditions.
Functional impact assessment is perhaps the most critical component. Examiners need to clearly explain how plantar fasciitis limits ability to work, exercise, and perform daily activities.
DBQ Completion Checklist:
- Qualified examiner familiar with VA criteria
- Detailed symptom frequency documentation
- Standardized pain scale measurements
- Range of motion assessments
- Functional limitation descriptions
- Treatment history review
- Work impact documentation
- Daily activity restrictions noted
Establishing Service Connection
Veterans must establish a clear link between military service and plantar fasciitis development through direct injury, repetitive stress, or aggravation of pre-existing conditions. This service connection forms the foundation for any disability rating consideration and requires specific types of evidence.
Service connection serves as the gateway to VA disability benefits. Without it, even severe plantar fasciitis won’t qualify for compensation. The evidence must demonstrate the condition relates to military service.
The VA recognizes several pathways to establish service connection for plantar fasciitis. Direct service connection is the most straightforward, but secondary service connection and aggravation claims are also possible.
Direct Service Connection Pathways
Direct service connection can be established through documented foot injuries during service, medical records showing plantar fasciitis diagnosis while on active duty, or clear evidence of condition onset during military service with continuous symptoms since discharge.
Direct service connection means plantar fasciitis started during military service or resulted from a specific service-related incident. This often represents the clearest path to benefits, though it requires solid documentation.
Documented foot injuries during service provide strong evidence for direct service connection. Service medical records showing foot injuries from training accidents, deployments, or any service-related activities can support claims.
Medical records showing plantar fasciitis diagnosis while on active duty create a clear timeline linking the condition to military service. Even if symptoms were mild initially, this documentation establishes the foundation for claims.
Continuous symptoms since discharge help bridge the gap between military service and current conditions. The VA reviews whether plantar fasciitis has persisted since service ended, rather than developing years later from unrelated causes.
Bilateral Plantar Fasciitis Considerations
When plantar fasciitis affects both feet, the VA applies bilateral factor calculations that can increase overall disability ratings beyond simple addition. Understanding these calculations and proper documentation requirements is important for accurate compensation.
Bilateral plantar fasciitis—affecting both feet—qualifies for additional compensation through the VA’s bilateral factor. This calculation differs from simple doubling and provides more comprehensive recognition.
The bilateral factor recognizes that having the same condition in both paired extremities creates additional functional limitations beyond what would be experienced with just one affected foot.
Understanding Bilateral Factor Application
The VA uses a specific mathematical formula for bilateral conditions affecting paired extremities, which can result in higher combined ratings than simply adding individual foot ratings together. This calculation method acknowledges the compounded disability impact of bilateral conditions.
The bilateral factor calculation works differently than straightforward addition. The VA doesn’t simply double ratings or add two separate ratings together.
Instead, the VA first determines individual ratings for each foot, combines them using the standard combined rating formula, then adds 10% of that combined value as the bilateral factor.
For example, if each foot rates 20%, the combined rating would be 36% (not 40%), and the bilateral factor would add another 3.6%, rounding to 40% total.
Combined Rating Calculations Explained
For bilateral plantar fasciitis, the VA first determines individual ratings for each foot, then applies the bilateral factor by adding 10% of the combined value to reach the final rating. This process requires separate medical documentation for each affected foot.
| Left Foot Rating | Right Foot Rating | Combined Rating | Bilateral Factor (10%) | Final Rating |
| 10% | 10% | 19% | 1.9% | 21% (rounded to 20%) |
| 20% | 20% | 36% | 3.6% | 40% |
| 20% | 30% | 44% | 4.4% | 48% (rounded to 50%) |
| 30% | 30% | 51% | 5.1% | 56% (rounded to 60%) |
The mathematics behind bilateral ratings can seem complex, but understanding the process shows why proper documentation for each foot matters.
First, the VA rates each foot individually based on its specific symptoms and limitations. The left foot might rate 20% while the right foot rates 30%, depending on severity differences.
Next, these ratings combine using the VA’s standard formula. This isn’t simple addition—the VA uses a formula that prevents combined ratings from exceeding 100%.
Finally, the bilateral factor applies by adding 10% of the combined rating value. This recognizes the additional functional impact of having both feet affected.
Documentation Strategies for Bilateral Cases
Bilateral cases require independent medical evaluation of each foot, including separate range of motion measurements, pain assessments, and functional limitation documentation. Medical professionals must clearly distinguish between left and right foot symptoms and limitations.
Documenting bilateral plantar fasciitis requires treating each foot as a separate condition, even though they’re related. Medical examiners need to evaluate and document each foot independently.
Range of motion measurements should be taken for both feet separately. Feet aren’t always equally affected—one foot might show more severe limitations than the other.
Pain assessments need to distinguish between left and right foot symptoms. Different pain levels, patterns, or triggers in each foot should be documented.
Functional limitation documentation should explain how each foot contributes to overall disability. Perhaps the right foot causes more morning pain while the left foot creates more difficulty during prolonged standing.
Army veteran James T. developed bilateral plantar fasciitis after years of carrying heavy equipment during deployments. His left foot rated 20% due to moderate morning pain and stiffness, while his right foot rated 30% because of severe pain requiring orthotic devices and activity modifications. Using the bilateral factor calculation: the combined rating of 44% plus the bilateral factor of 4.4% resulted in a final rating of 50%, significantly higher than unilateral plantar fasciitis would have provided.

Claim Filing Strategies and Processes
Successfully navigating plantar fasciitis disability benefits requires understanding different claim types, timing considerations, and evidence requirements. Veterans can pursue initial claims for unrated conditions or increase claims for worsening symptoms, each requiring different documentation approaches.
Filing plantar fasciitis claims varies based on whether veterans are seeking first-time ratings for this condition or requesting increases for existing ratings that no longer reflect current symptoms.
Timing significantly impacts outcomes. When claims are filed, what evidence is submitted, and how cases are presented can affect results. .
Initial Claims vs. Increase Claims
Understanding the difference between initial claims and increase claims is important for veterans pursuing plantar fasciitis benefits through appropriate channels.
Veterans file initial claims when seeking their first rating for plantar fasciitis. These claims start from the beginning, requiring establishment of service connection, current diagnosis, and disability severity all at once.
Increase claims apply when veterans already have plantar fasciitis ratings but believe current ratings don’t reflect how much worse their conditions have become. Understanding the VA disability rating increase process can clarify these procedures.
Initial Claim Requirements
Initial claims require establishing service connection, current diagnosis, and nexus between military service and condition development. Veterans must provide comprehensive medical evidence showing plantar fasciitis exists and relates to military service.
Initial claims need to establish three elements: service connection, current diagnosis, and nexus (the link between military service and current conditions).
Service connection evidence might include service medical records, incident reports, or buddy statements describing when and how plantar fasciitis developed during military service.
Current diagnosis requires recent medical records confirming plantar fasciitis currently exists. The VA won’t rate conditions that existed years ago but no longer occur.
Nexus evidence connects current plantar fasciitis to military service. This might include medical opinions from doctors explaining how service activities caused or aggravated the condition.
Initial Claim Documentation Checklist:
- Service medical records
- Current medical diagnosis
- Medical opinion linking service to condition
- Service incident reports (if applicable)
- Buddy statements from fellow service members
- DD-214 or service records
- Complete DBQ evaluation
- Treatment history documentation
Increase Claim Procedures
Increase claims focus on demonstrating worsening symptoms since the last rating decision. Veterans must provide updated medical evidence showing progression of plantar fasciitis symptoms and increased functional limitations compared to previous evaluations.
Increase claims center on showing progression. The VA needs to see that plantar fasciitis has worsened since the last rating decision.
Updated medical evidence should clearly document how symptoms have changed. Pain may have increased, functional limitations may have expanded, or treatments that previously helped may no longer be effective.
Comparative documentation helps illustrate progression. When possible, referencing previous examination findings and showing how current conditions differ strengthens increase claims.
New treatment attempts or failures can support increase claims. If additional treatments have been tried since the last rating without success, this demonstrates worsening severity.
Evidence Development and Medical Examinations
Strong medical evidence forms the foundation of successful plantar fasciitis claims, requiring coordination between veterans, medical professionals, and understanding of VA evaluation standards. Proper evidence development can significantly impact claim outcomes.
Building strong evidence foundations takes time and coordination. Single doctor’s appointments rarely provide everything needed for successful claims.
The quality of medical examinations matters more than quantity. One comprehensive evaluation by a knowledgeable provider outweighs multiple superficial examinations.
Independent Medical Evaluations
Independent medical evaluations provide objective, comprehensive assessments of plantar fasciitis severity and functional impact. These evaluations can supplement VA examinations and provide additional evidence for rating decisions.
Independent medical evaluations offer several advantages over standard medical appointments. Examining physicians focus specifically on documenting conditions for disability purposes rather than only treating symptoms.
These evaluations typically include comprehensive functional assessments that measure exactly how plantar fasciitis limits daily activities. This objective data carries significant weight in rating decisions.
Independent examiners often have experience with VA rating criteria and understand what documentation the VA needs to make accurate rating decisions.
Treatment History Documentation
Complete treatment records demonstrate condition severity and response to various interventions, including conservative treatments, physical therapy, injections, and surgical procedures. Failed treatments often support higher disability ratings.
Treatment history tells the story of plantar fasciitis progression. The VA wants to see what treatments have been attempted and how well they’ve worked.
Conservative treatments like rest, ice, stretching, and over-the-counter medications are usually first-line interventions. Documenting these attempts, even if they seem minor, provides valuable context.
Physical therapy records show serious efforts to improve the condition. If PT didn’t provide lasting relief, this supports claims of persistent disability.
Injection treatments and surgical procedures indicate severe symptoms that haven’t responded to conservative care. Failed invasive treatments often support higher disability ratings.
The importance of proper footwear and support in managing plantar fasciitis has gained attention, with podiatrists recommending specific features like arch support and cushioning. According to SELF Magazine, when managing plantar fasciitis, medical experts emphasize the importance of arch support in footwear, with proper heel cups and elevated heel-to-toe drops helping reduce pressure on the plantar fascia.

Common Documentation Issues and How to Address Them
Many veterans receive lower plantar fasciitis ratings due to incomplete medical documentation, inadequate symptom reporting, or failure to establish proper service connection. Understanding these common challenges helps veterans prepare stronger claims from the outset.
Veterans often make predictable errors that affect disability benefits. Learning from common issues can save time, frustration, and improve outcomes.
The most significant challenges often happen early in the process. Once low ratings are received based on insufficient evidence, increasing them later becomes more difficult.
Insufficient Medical Evidence
Incomplete medical records, lack of objective testing, and inadequate functional capacity assessments frequently result in lower ratings. Veterans must work with medical providers to document all aspects of their conditions using VA-recognized assessment methods and terminology.
Insufficient medical evidence is among the most common reasons veterans receive lower ratings than their conditions warrant. The VA can only rate what’s documented in medical records.
Incomplete medical records leave gaps that may be interpreted less favorably. Missing treatment records, incomplete examination findings, or vague symptom descriptions all affect claims.
Lack of objective testing weakens cases significantly. Subjective complaints carry less weight than objective measurements, imaging results, and standardized assessments.
Inadequate functional capacity assessments fail to show the VA how plantar fasciitis actually limits daily activities. General statements about pain don’t demonstrate specific functional restrictions.
Inadequate Symptom Reporting
Veterans often underreport symptoms during medical examinations, leading to ratings that don’t reflect true functional limitations. Honest, detailed reporting of worst-case scenarios and daily challenges provides more accurate assessment of disability severity.
Many veterans minimize symptoms during medical examinations. Military culture often emphasizes pushing through pain rather than reporting it, but this mindset can affect disability claims negatively.
Underreporting symptoms leads to ratings that don’t reflect true functional limitations. When veterans describe pain as “manageable,” higher disability ratings become less likely.
Honest reporting about worst days provides more accurate disability assessment. The VA needs to understand how plantar fasciitis affects veterans when symptoms are severe, not only on best days.
Detailed descriptions of daily challenges help examiners understand functional impact. Instead of general statements like “my feet hurt,” specific explanations of how pain affects work, sleep, exercise, and daily activities provide clearer pictures.
Service Connection Documentation Gaps
Failure to establish clear nexus between military service and plantar fasciitis development frequently leads to claim denials. Veterans must provide comprehensive service records, buddy statements, and medical opinions linking their conditions to military activities or injuries.
Service connection gaps cause more claim denials than any other factor. Without clear connection to military service, even severe plantar fasciitis won’t qualify for VA benefits.
Missing service records make it impossible to establish when and how plantar fasciitis developed. Incomplete personnel files, lost medical records, or missing incident reports all create documentation gaps.
Lack of buddy statements leaves claims without witness testimony about condition development during service. Fellow service members can provide important evidence about incidents or symptoms they observed.
Absent medical opinions fail to connect current conditions to military service. Even with service records and current diagnoses, medical professionals often need to explain the connections.
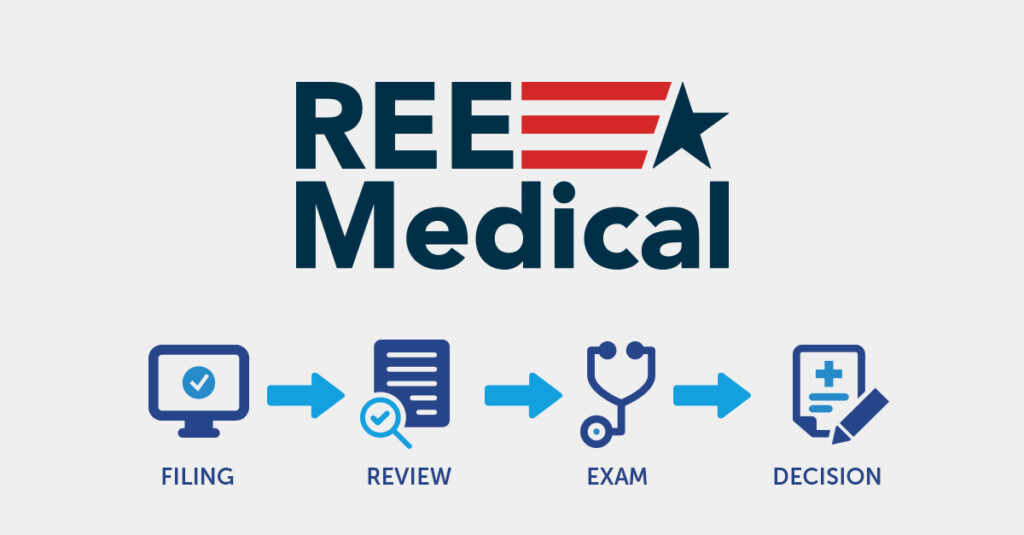
How REE Medical Supports Veterans with Plantar Fasciitis Documentation
REE Medical coordinates independent medical evaluations that provide veterans with comprehensive, VA-compliant documentation for plantar fasciitis claims. Through a nationwide network of licensed medical professionals who specialize in disability-focused documentation, REE Medical connects veterans with qualified physicians who understand the specific requirements for plantar fasciitis DBQs.
The coordination process begins with a complimentary consultation to explain how independent medical documentation is developed. REE Medical’s staff coordinates access to licensed healthcare professionals familiar with VA-standardized forms and disability-focused documentation requirements.
Independent evaluations coordinated through REE Medical provide detailed, objective clinical documentation that meets VA formatting standards. These evaluations include comprehensive functional assessments that measure how plantar fasciitis affects daily activities, work capacity, and quality of life.
Veterans can learn more about coordinating VA-compliant DBQs and independent medical evaluations by contacting REE Medical for an informational consultation. REE Medical’s team explains the documentation coordination process and connects veterans with independent, licensed medical providers.
Final Thoughts
Plantar fasciitis might seem straightforward, but accurate VA ratings require understanding the system’s complexities and documentation requirements. Ratings depend on much more than heel pain—the VA needs comprehensive evidence showing exactly how this condition limits daily functioning and connects to military service.
The difference between rating levels can mean hundreds of dollars monthly for decades. Whether pursuing initial claims or seeking increases, thorough documentation and working with knowledgeable medical professionals is important. Insufficient evidence can significantly affect the benefits veterans have earned through their service.
Bilateral plantar fasciitis qualifies for additional compensation through the bilateral factor, and strategic timing of medical evaluations can impact outcomes. Honest, detailed reporting of worst symptoms provides the most accurate assessment of disability severity.

Disclosure
DISCLAIMER: REE Medical, LLC is not a Veterans Service Organization (VSO) or a law firm and is not affiliated with the U.S. Veterans Administration (“VA”). Results are not guaranteed, and REE Medical, LLC makes no promises. REE Medical’s staff does not provide medical advice or legal advice, and REE Medical is not a law firm. Any information discussed, such as, but not limited to, the likely chance of an increase or service connection, estimated benefit amounts, and potential new ratings, is solely based on past client generalizations and not specific to any one patient. The doctor has the right to reject and/or refuse to complete a Veteran’s Disability Benefit Questionnaire if they feel the Veteran is not being truthful. The Veteran’s Administration is the only agency that can make a determination regarding whether or not a Veteran will receive an increase in their service-connected disabilities or make a decision on whether or not a disability will be considered service-connected. This business is not sponsored by, or affiliated with, the United States Department of Veterans Affairs, any State Department of Military and Veterans Affairs, or any other federally chartered veterans service organization.