VA Rating for Depression: What Many Veterans Wish They Knew About VA Evaluation
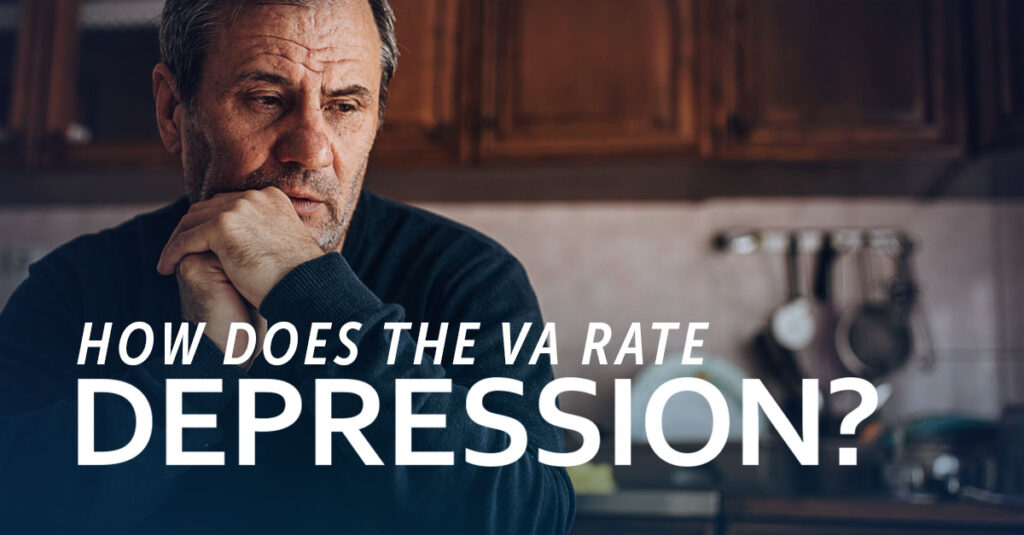
If you’re reading this, chances are you’re dealing with depression related to your military service. You are not alone. Way too many veterans struggle with depression symptoms. VA estimates show that approximately 1 in 3 (33.3%) of Veterans have some symptoms of depression, 1 in 5 (20%) have serious symptoms, and 1 in 8 (12.5%) have major depression requiring treatment with psychotherapy and antidepressants, according to “VA Disability Rating for Depression” by Hill & Ponton. Understanding the criteria the VA uses to determine disability ratings for depression can help veterans understand what to expect during the VA’s evaluation process.
TL;DR
- The VA focuses on how badly depression affects work and social life rather than what type of depression exists
- Medical evidence needs to show exactly how depression limits daily functioning – general statements about feeling depressed aren’t enough
- Depression and anxiety usually get rated together since symptoms overlap so much
- Most veterans end up with ratings between 30-70%, depending on documentation
- The VA may schedule a Compensation and Pension (C&P) exam when existing medical evidence needs clarification
- Sometimes regular medical records don’t tell the complete story. Independent medical documentation can provide comprehensive functional assessments
The Reality Check: How the VA Actually Rates Depression
The VA’s evaluation process focuses on functional impairment rather than depression type. Major depression, general depression, and seasonal depression all receive evaluation under the same criteria. The VA examines how symptoms affect work ability, relationships, and daily tasks.
The VA’s focus on functional impairment means that similar diagnoses may receive different ratings based on how thoroughly medical records document limitations. Two veterans with comparable symptoms may receive different ratings depending on the quality and completeness of their medical documentation.

The One-Size-Fits-All Mental Health System
The VA applies identical rating criteria across depression, PTSD, anxiety, and other mental health conditions. These criteria derive from the Diagnostic and Statistical Manual for Mental Disorders, Fifth Edition (DSM-5) published by the American Psychiatric Association (APA) to rate all mental health conditions, as noted in “VA Disability Rating for Depression and Anxiety” by CCK Law.
Rating percentages follow specific increments: 0%, 10%, 30%, 50%, 70%, and 100%. Each level corresponds to detailed criteria related to occupational and social impairment. The VA reviews medical evidence to identify documentation matching these criteria. Medical records must document specific functional limitations rather than general symptom descriptions.
| Rating | Monthly Compensation (2025) | What This Actually Means |
| 0% | $0.00 | Diagnosis present but minimal functional impact |
| 10% | $175.51 | Mild symptoms during stress, generally controlled by medication |
| 30% | $537.42 | Occasional inability to work, periodic relationship difficulties |
| 50% | $1,102.04 | Frequent work absences, panic attacks, relationship problems |
| 70% | $1,759.19 | Severe functional impairment, suicidal ideation, pervasive difficulties |
| 100% | $3,831.30 | Total occupational and social impairment |
Source: “VA Disability Rating for Depression” by Eisenberg Law Office
What the VA Evaluates
The VA examines specific functional areas when determining ratings. Employment stability, workplace performance, relationship functioning, and ability to handle routine daily tasks all factor into the evaluation. Panic attacks during work, deteriorating relationships due to mood changes, self-care difficulties, and stress management challenges all represent relevant functional limitations.
Medical documentation requires specific examples rather than generic statements. Documentation stating “patient reports feeling depressed” provides insufficient detail for VA evaluation. Records showing missed workdays, relationship problems, self-care difficulties, or stress-response impairment provide more substantial evidence.
Consider this example: A veteran with a 50% rating has medical records documenting 2-3 monthly work absences due to inability to function, relationship dissolution attributed to emotional withdrawal, family assistance required for grocery shopping during severe episodes, and panic attacks during workplace team meetings. These concrete examples of functional limitations allow the VA to evaluate the condition’s impact accurately.
When Depression Occurs with Anxiety
Many veterans experience both depression and anxiety simultaneously. The VA typically combines ratings for these conditions under one percentage rather than separating them. This combined approach reflects the significant symptom overlap between depression and anxiety, making isolation of individual condition impacts nearly impossible.
The combined rating approach can benefit veterans. Rather than receiving separate lower ratings for each condition, veterans may receive one higher rating covering all combined mental health symptoms and their cumulative functional impacts.
Understanding Your Claim Options
VA claims for depression involve strategic documentation and timing considerations. The type of claim—initial, increase, or secondary—determines specific requirements. Understanding these distinctions clarifies the evaluation process.

Your First Claim: Starting From Zero
Initial claims establish service connection for the condition. The VA requires three elements: current depression diagnosis, military service event or exposure contributing to the condition, and medical evidence connecting the current condition to service. Missing documentation of any element results in claim denial.
Common errors include submitting claims before medical evidence is complete. Incomplete initial submissions may face extended processing times or require additional evidence requests. Initial VA evaluations rely on evidence such as service and post-service treatment records, which the VA reviews during the decision process.
As noted in “VA Disability Rating for Depression and Anxiety” by CCK Law, service connection requires three basic elements: a current diagnosis, evidence of an in-service event, injury, or illness, and a medical connection (independent medical opinion linking the current diagnosed condition to the in-service occurrence). Depression claims differ from PTSD claims in not requiring establishment of a specific “stressor” event.
Understanding initial claims clarifies appropriate approaches for first-time filers.
Seeking Rating Increases
Veterans with existing ratings may seek increased compensation when conditions worsen. Increase claims require medical evidence documenting symptom and functional limitation deterioration since the previous rating decision.
Timing affects benefit effective dates and potential retroactive payments. The VA backdates higher ratings to increase claim filing dates, making earlier filing financially beneficial. However, premature filing without established worsening patterns can complicate claims. The VA generally evaluates whether documentation reflects sustained patterns of symptom change over time.
Consider this example: A veteran initially rated at 30% experiences significant deterioration two years later. Updated documentation shows work absences increasing from 1-2 to 4-5 monthly, therapy frequency increasing from monthly to three times weekly, daily panic attacks versus previous weekly occurrence, and two hospitalizations for suicidal ideation. When psychiatric documentation provides detailed comparison to previous functioning levels, ratings may increase from 30% to 70% with retroactive compensation to the filing date.
Veterans can learn about VA disability rating increases to understand specific requirements.
What Most Veterans Actually Receive
While VA ratings span 0% to 100%, most veterans receive ratings in the 30-70% range. According to “VA Disability Rating for Depression” by Hill & Ponton, 30% represents the most common depression rating.
This pattern reflects moderate impairment documentation rather than restricted compensation. Most properly documented depression cases demonstrate moderate functional limitation levels. Individual ratings depend entirely on medical evidence quality documenting functional limitations matching VA rating criteria. Comprehensive medical documentation that describes how depression affects various aspects of life helps the VA make a thorough evaluation.
Rating differences between 30% and 70% often stem from documentation quality rather than symptom severity alone. Veterans whose mental health providers understand VA requirements typically receive more accurate ratings because their medical records include the specific functional assessments the VA evaluates.
Accurate Medical Evidence That Actually Works
Strong medical evidence results from working with mental health providers who understand VA evaluation requirements. Treatment records should comprehensively describe how depression affects all life aspects, extending beyond clinical symptom summaries and medication lists.
Effective medical evidence includes specific functional limitation examples, detailed symptom severity descriptions, and clear documentation of real-world problems caused by depression. Generic treatment notes applicable to any patient provide insufficient support for accurate VA evaluation.
Working with Knowledgeable Providers
Not all mental health providers understand VA documentation requirements, potentially resulting in ratings not reflecting actual impairment levels. Veterans benefit from providers who document symptoms and their translation into work problems, relationship difficulties, and daily activity limitations.
Initial VA evaluations rely on evidence such as service and post-service treatment records, which the VA reviews during the decision process. Most providers welcome this information but may not initially understand specific VA documentation requirements.
Understanding the importance of medical evidence in VA disability claims demonstrates why detailed documentation matters significantly.
Documenting Functional Impact
The VA evaluates functional impact rather than emotional experiences. Medical records require specific examples showing how depression prevents employment maintenance, causes relationship problems, or interferes with self-care.
Work-related functional limitations deserve particular attention since job performance significantly influences VA ratings. The VA considers documentation describing work absences, concentration difficulties, or interpersonal challenges when determining functional impact. Employment losses or hour reductions due to depression warrant medical record inclusion.
| What to Document | Specific Examples |
| Work Problems | “Missed 15 days in 3 months because couldn’t get out of bed” |
| Relationship Issues | “Ended 5-year relationship due to emotional withdrawal and mood swings” |
| Daily Life Struggles | “Family has to help with grocery shopping during bad episodes” |
| Mental Function | “Can’t focus during meetings, loses train of thought constantly” |
| Sleep Problems | “Sleeps 12-14 hours daily but still feels exhausted and unmotivated” |
When Regular Records May Be Insufficient
Existing medical records may not fully document how depression affects daily functioning. Providers may not document functional limitations thoroughly, or treatment gaps may exist. Documentation gaps may require additional medical clarification before the VA can make a full determination.
Independent medical evaluations provide comprehensive assessments that the VA may use to better understand a veteran’s condition. These evaluations focus on functional limitations and include detailed documentation about how depression affects work ability and social functioning.

The VA May Require a C&P Exam for Your Claim
When the VA requires additional information beyond submitted medical records, they may schedule a Compensation and Pension (C&P) Examination as described by VA.gov.
REE Medical coordinates independent medical evaluations and DBQs that provide comprehensive documentation for VA review. Thorough independent documentation may reduce the likelihood of additional VA examination requirements.
Understanding common reasons for VA claim denials helps clarify how documentation is evaluated.

What to Expect and When Professional Documentation Can Help
Understanding realistic timelines and potential outcomes supports appropriate expectation management throughout the evaluation process. Depression claims often require longer processing than physical disability claims because documenting psychological symptoms and functional limitations involves more complex evaluation.
Timeline Realities
Mental health claims typically process more slowly than physical condition claims. Initial claims generally take 4-8 months, though duration varies significantly based on regional office workload and case complexity.
Increase claims often process faster since service connection already exists. However, adequate time for developing medical evidence showing sustained worsening precedes filing. Increase requests submitted without sufficient supporting evidence may take longer to process or require additional review.
Appeals and higher-level reviews extend processing timelines but may prove necessary for achieving accurate ratings. Appeals represent essential evaluation process steps rather than failures, often crucial for fair compensation determination.
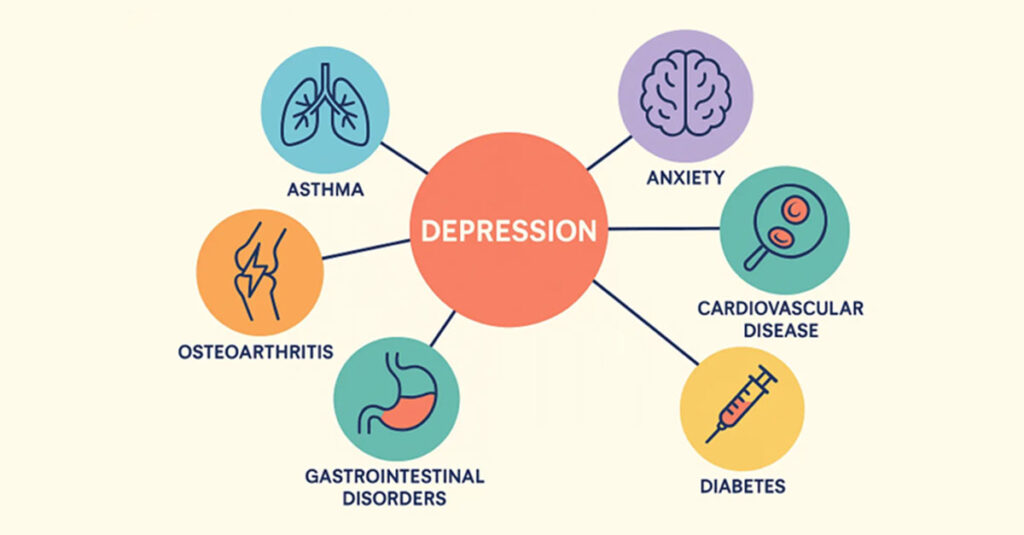
Secondary Conditions That Affect Overall Ratings
Depression rarely exists in isolation. Related conditions including anxiety, sleep disorders, chronic pain, or substance concerns often develop alongside or result from depression. These secondary conditions can affect overall disability compensation through the VA’s combined rating formula.
Recognition of connections between depression and other service-connected conditions continues increasing. According to “Erectile Dysfunction and Depression” by Hill & Ponton, depression frequently links to other health issues as a secondary condition. Veterans experiencing depression often face decreased sexual desire and diminished intimate connection capacity, potentially resulting in erectile dysfunction among other concerns.
Medical documentation of connections between depression and other health problems strengthens claims. Depression causing insomnia, chronic pain worsening depression, and similar relationships can result in additional disability ratings substantially increasing overall compensation.
Any condition related to or caused by a service-connected condition may also receive service connection consideration, even without occurrence during active service.
When Professional Medical Documentation Makes Sense
Several situations make independent medical evaluations particularly valuable for depression claims. When current treatment records lack detailed functional assessments, or when existing ratings don’t reflect actual impairment levels, comprehensive independent medical documentation can strengthen cases.
Veterans without consistent mental health treatment often benefit significantly from independent evaluations. These assessments can establish baseline documentation of condition severity and functional impact even without extensive treatment history.
Recent developments may impact future depression claims. According to “Vets’ disability benefits for tinnitus, mental health issues may change” by Military Times, proposed VA disability rating system changes would create lower thresholds for veterans with mental health conditions to receive increased disability ratings.
Veterans can learn about evidence requirements for disability claims to understand how professional documentation services may complement their overall approach.
How REE Medical Coordinates Independent Evaluations
Veterans whose current medical records don’t fully document depression’s impact on their lives may benefit from comprehensive independent evaluations. REE Medical coordinates connections between veterans and independent healthcare providers specializing in VA disability evaluations.
REE Medical coordinates independent medical evaluations meeting VA standards for disability claims. Their network of qualified mental health providers understands specific VA documentation requirements and effective presentation of functional limitation evidence.
Flat-rate pricing eliminates cost surprises and focus on functional limitation documentation addresses specific criteria the VA uses for rating determinations. For veterans whose existing medical records don’t fully capture depression’s impact, REE Medical’s coordination services can address critical documentation gaps.
Detailed evaluations that compare current functioning to previous rating levels can provide the VA with clearer insight into changes over time. REE Medical’s providers understand how depression symptoms align with VA rating criteria, positioning them to document evidence most relevant for disability claims.
REE Medical connects veterans with independent, licensed medical professionals who complete thorough, accurate Disability Benefit Questionnaires (DBQs). REE Medical does not prepare, present, or prosecute VA disability claims; the Department of Veterans Affairs makes all rating determinations.
Final Thoughts
Achieving accurate VA ratings for depression involves understanding complex evaluation requirements. Knowledge of service connection elements, strategic timing considerations, and proper medical evidence standards provides veterans with a foundation for navigating the benefits process.
VA disability compensation reflects military service and resulting conditions. Through thorough preparation, comprehensive medical evidence, and understanding of VA evaluation criteria, veterans can navigate the disability system more effectively.
The process requires time and persistence, but accurate disability compensation benefits justify the effort. Every veteran experiencing post-service depression has earned the right to seek fair compensation through the VA system.
The key lies in approaching claims strategically, gathering comprehensive medical evidence, and understanding how the VA evaluates functional impairments. Veterans have served their country; accurate ratings reflect that service and its lasting impacts.
Many of the same principles that apply to PTSD evaluations also apply to depression, offering helpful context for understanding the VA system.
Veterans seeking comprehensive medical documentation for depression claims can learn how REE Medical coordinates connections with qualified healthcare providers who understand VA requirements and document service-connected conditions thoroughly. Contact REE Medical for an informational consultation about coordinating independent medical documentation.
DISCLAIMER
REE Medical, LLC is not a Veterans Service Organization (VSO) or a law firm and is not affiliated with the U.S. Veterans Administration (“VA”). Results are not guaranteed, and REE Medical, LLC makes no promises. REE Medical’s staff does not provide medical advice or legal advice, and REE Medical is not a law firm. Any information discussed, such as, but not limited to, the likely chance of an increase or service connection, estimated benefit amounts, and potential new ratings, is solely based on past client generalizations and not specific to any one patient. The doctor has the right to reject and/or refuse to complete a Veteran’s Disability Benefit Questionnaire if they feel the Veteran is not being truthful. The Veteran’s Administration is the only agency that can make a determination regarding whether or not a Veteran will receive an increase in their service-connected disabilities or make a decision on whether or not a disability will be considered service-connected. This business is not sponsored by, or affiliated with, the United States Department of Veterans Affairs, any State Department of Military and Veterans Affairs, or any other federally chartered veterans service organization.