PTSD DBQ: What Veterans Should Know About Disability Benefits Questionnaires
The PTSD Disability Benefits Questionnaire (DBQ) represents a critical piece of medical evidence in VA disability evaluations. Approximately 7% of veterans develop PTSD at some point in their lives, according to VA Claims Insider, making comprehensive medical documentation essential for accurate disability assessments. This overview explains how DBQs function within the VA evaluation process and what medical evidence the VA reviews when assessing PTSD claims.
Key Takeaways
- The PTSD DBQ serves as critical medical evidence that the VA reviews during disability evaluations
- Military Sexual Trauma (MST) cases often require alternative evidence sources due to limited service records
- Initial claims require comprehensive DSM-5 criteria documentation and clear service connection evidence
- Increase claims benefit from documentation showing condition changes since the last VA rating decision
- Proper DBQ completion requires specific VA terminology and formatting standards
- For treatment-resistant PTSD cases, documentation showing multiple intervention attempts can help the VA understand symptom history and clinical context.
- Comorbid conditions require careful clinical documentation that addresses each condition separately
Understanding PTSD Disability Benefit Questionnaires
The PTSD DBQ serves as a standardized medical document that the VA uses to evaluate disability claims. This form translates clinical findings into the specific criteria that VA raters use when assigning disability percentages. Understanding how DBQs function within the VA system helps veterans recognize the type of medical evidence the VA considers during claim evaluations.
The VA uses more than one type of PTSD-related Disability Benefits Questionnaire. For first-time PTSD disability claims, the VA generally relies on an internal Initial PTSD DBQ that is completed by a VA clinician during a Compensation & Pension (C&P) examination. This VA-only form is not publicly available. Independent, non-VA providers may complete PTSD-related DBQs or other clinical documentation that can supplement the record—particularly for review and rating increase purposes—but these do not replace the VA’s Initial PTSD DBQ for initial PTSD claims.
The Foundation of PTSD Disability Claims
Every PTSD disability claim involves medical documentation that captures symptom severity and functional impairment. The VA uses this documentation to assign disability ratings based on how conditions affect occupational and social functioning. The PTSD DBQ follows a comprehensive format aligned with DSM-5 standards while addressing VA-specific rating criteria.
The PTSD DBQ differs from standard psychiatric evaluations because it captures specific information the VA needs for rating decisions. The current form structure addresses four critical areas: diagnostic criteria, symptom severity, functional limitations, and service connection evidence.
Breaking Down the Current PTSD DBQ Structure
The latest PTSD DBQ evaluates conditions against specific VA rating percentages, from 0% to 100%, based on occupational and social impairment levels. The VA assesses how symptoms affect daily life, work capacity, and social functioning rather than simply confirming symptom presence.
Modern VA DBQ forms incorporate DSM-5 updates while maintaining the VA’s unique rating approach. This creates a bridge between clinical psychology and disability law that requires specialized documentation knowledge.
Medical Evidence the VA Reviews
The VA reviews comprehensive medical evidence when evaluating PTSD claims. This includes documented diagnosis, detailed symptom chronology, and clear connection to military service or qualifying traumatic events. The quality and specificity of this evidence influences the VA’s evaluation outcomes.
Medical evidence needs to trace PTSD from the traumatic military event through current symptoms. The VA reviews documentation showing how symptoms developed, what treatments were attempted, and how symptoms affect work ability, relationships, and social functioning.
Aligning Symptoms with VA Rating Criteria
DBQ responses correspond to VA rating percentages through specific language about occupational and social impairment levels. Clinical documentation needs to align with rating schedules using terminology that describes functional limitations rather than just symptom presence.
The rating criteria focus on functional capacity rather than symptom intensity. The VA may assign different ratings to veterans with similar symptom severity based on how those symptoms affect their ability to work and function socially.
PTSD DBQ for Military Sexual Trauma Cases
MST-related PTSD claims present unique documentation challenges due to limited service records. These cases often require alternative evidence sources and trauma-informed assessment protocols that account for reporting barriers and memory considerations during evaluation.
Military Sexual Trauma cases demand specialized documentation approaches. Traditional service records often don’t exist for MST incidents, creating challenges that require alternative evidence gathering techniques.
According to VA Claims Insider, about 1 in 3 women veterans and 1 in 50 male veterans report experiencing MST when screened by their VA provider, highlighting the significant prevalence of this trauma type among veterans seeking disability benefits.
Overcoming MST Documentation Obstacles
MST claims frequently lack traditional service records, requiring alternative evidence sources like contemporaneous medical records, behavioral change documentation, and witness statements from service members who observed changes during or after the trauma period.
The absence of official incident reports doesn’t preclude MST claims, but it requires strategic evidence development. Alternative indicators may include medical treatment for physical symptoms during service, performance evaluation changes, or documented behavioral changes observed by family members or colleagues.
MST Evidence Development Example: A female Navy veteran filed for PTSD related to sexual assault during deployment. With no official incident report, the VA ultimately granted service connection based on medical records showing treatment for physical symptoms shortly after the incident, a performance evaluation noting behavioral changes during the same period, and family statements documenting personality changes upon return from deployment. In this example, the DBQ documented how these indirect indicators related to the reported MST, and the VA considered that documentation along with the rest of the evidence when determining service connection.
Trauma-Informed Assessment Approaches
Medical professionals conducting MST evaluations employ sensitive questioning methods that prevent re-traumatization while gathering necessary clinical information. These evaluations often require multiple sessions and specialized interview techniques that differ from standard clinical protocols.
The trauma-informed approach recognizes that discussing sexual trauma can trigger symptoms and requires modified techniques that prioritize psychological safety while gathering necessary medical information. Effective MST DBQs often involve multiple evaluation sessions, allowing trust development between the examiner and veteran.

PTSD Review and Re-evaluation DBQs
Review DBQs address changing symptoms, treatment responses, and functional capacity fluctuations over time. These evaluations document both improvement and deterioration patterns while considering treatment compliance and effectiveness measures.
PTSD symptoms change over time, and review DBQs capture these changes for the VA’s consideration. These evaluations require different documentation approaches than initial claims because they address condition evolution rather than initial diagnosis establishment.
Documenting Symptom Evolution Over Time
Review DBQs capture longitudinal symptom patterns, including treatment compliance, medication effectiveness, and functional capacity changes. This provides a comprehensive picture of condition trajectory since the last evaluation.
Symptom progression documentation requires careful attention to timeline and causation. The VA considers whether symptoms worsened due to life stressors or despite consistent treatment, and whether new symptoms emerged or existing symptoms intensified.
Treatment compliance becomes a factor in review DBQ evaluations. The VA reviews whether symptom persistence reflects treatment resistance or other factors, which can affect rating determinations.
Initial PTSD DBQ Documentation (Completed by VA Examiners)
For first-time PTSD disability claims, the VA typically relies on an Initial PTSD DBQ completed by VA clinicians as part of its internal C&P examination process. This VA-only form establishes foundational medical evidence for the initial claim. These evaluations require comprehensive diagnostic assessment that meets DSM-5 criteria while establishing clear service connection through chronological documentation and baseline functional assessment.
The initial PTSD DBQ creates the medical record foundation for disability claims. This documentation establishes condition severity, service connection, and functional impact.
Establishing PTSD Diagnosis
Initial claims require formal PTSD diagnosis meeting DSM-5 criteria with clear documentation of qualifying traumatic events, symptom onset timing, and comprehensive evaluation of pre-military, military, and post-military functioning.
PTSD diagnosis for VA purposes requires establishing not just clinical criteria, but also service connection and significant functional impact. The initial DBQ needs to document all three elements comprehensively.
Meeting DSM-5 Documentation Standards
Medical professionals document all four DSM-5 criterion clusters: intrusion symptoms, avoidance behaviors, negative cognitions and mood alterations, and arousal and reactivity changes. Each category requires specific examples and functional impact assessments.
DSM-5 criteria provide the clinical framework, but evaluations need specific examples within each category. Instead of simply noting “intrusion symptoms,” effective documentation describes the frequency, intensity, and impact of nightmares, flashbacks, or intrusive thoughts.
Criterion A (trauma exposure) requires detailed documentation of the qualifying military traumatic event. Criteria B through E need functional impact documentation showing how avoidance behaviors, negative thoughts, hypervigilance, and other symptoms affect daily functioning.
Building Service Connection Evidence
Initial DBQs require clear linkage between military service events and PTSD development through medical opinions using specific probability language. Chronological documentation traces symptom development from service to present.
Service connection evidence establishes a clear timeline from military traumatic events to current PTSD symptoms. Medical opinion sections use specific probability language that the VA considers when making service connection determinations.
According to VA Claims Insider, veterans of Operations Iraqi Freedom and Enduring Freedom have PTSD rates of 15% experiencing symptoms in the past year and 29% at some point in their lives, making proper service connection documentation particularly important for OIF/OEF veterans.
Comprehensive Baseline Functional Assessment
Evaluation of pre-military, military, and post-military functioning establishes baseline capacity levels. This comparison between pre-trauma functioning and current capacity helps establish the degree of impairment the VA considers when assigning ratings.
Baseline functional assessment becomes the foundation for all future evaluations. Pre-military functioning documentation includes educational achievements, employment history, relationship patterns, and social activities, establishing baseline capacity before military trauma exposure.
Post-military functional assessment requires specific examples of impairment areas, including work performance changes, affected relationships, and activities discontinued due to PTSD symptoms.
Clinical Interview Standards for Initial Claims
When the VA conducts its own initial PTSD evaluation, proper Initial PTSD DBQ completion involves structured clinical interviews that capture symptom severity, frequency, and functional impact through specific examples and quantified measurements.
Clinical interviews for initial PTSD DBQs are structured evaluations designed to gather specific information for disability rating purposes. This differs from therapeutic sessions in its focus on documentation requirements.
Quantifying Symptom Severity
Clinicians document specific examples of symptom manifestation, including frequency, duration, and intensity measurements. This provides concrete evidence that supports specific disability rating percentages.
Symptom severity quantification requires specific metrics. Effective DBQs document nightmare frequency, duration, and resulting sleep disruption rather than general statements about sleep disturbance. Panic attack documentation includes frequency, duration, triggers, and functional impact.
Concentration difficulties benefit from specific examples showing how symptoms affect reading ability, task completion, and work performance. These concrete examples translate into functional limitation assessments.
Symptom Quantification Example: Instead of documenting “veteran experiences hypervigilance,” an effective DBQ states: “Veteran reports constant environmental scanning in public spaces, discomfort sitting with back to door in restaurants, repeated lock-checking behaviors, and leaving crowded stores due to anxiety. These behaviors prevent normal social activities and limit employment options.”

PTSD DBQ for Rating Increases
Increase claims utilize DBQs to document worsening PTSD symptoms or inadequate initial ratings. These claims compare current functioning against previously documented levels, requiring comprehensive evidence of deterioration or previously undocumented impairment.
PTSD symptoms can worsen over time, or initial ratings may not capture the full extent of impairment. Increase claims require different documentation than initial claims because they demonstrate condition changes rather than establishing initial diagnosis.
Documenting Worsening Conditions
Increase DBQs demonstrate clear deterioration in PTSD symptoms or functional capacity since the last VA rating decision. Documentation includes comparative analysis, treatment history, and detailed occupational impairment evolution.
Symptom deterioration documentation requires specific comparisons between current functioning and status at the time of the last rating decision. The VA considers this comparative evidence when evaluating increase claims.
Comparative Functional Analysis Strategies
Medical professionals compare current functioning against previous DBQ findings, highlighting specific areas of decline or newly emerged symptoms. Documentation includes failed treatment attempts and progressive functional limitations.
Comparative analysis needs to be methodical and specific. If previous documentation noted occasional panic attacks, increase documentation might show they’ve become daily occurrences affecting home confinement. This progression requires clear documentation with specific examples.
Employment history provides comparative evidence. Changes from full-time employment to inability to maintain work, demotions, terminations, or reduced hours due to worsening symptoms support increase claims.
Social functioning deterioration offers another comparison point. Withdrawal from family activities, discontinued hobbies, or ended friendships due to worsening symptoms support higher ratings.
Treatment History’s Impact on Increase Claims
Documentation includes treatment compliance, medication effectiveness, and therapy outcomes to establish how clinical picture has changed. This shows whether symptom worsening occurred despite appropriate treatment rather than due to non-compliance.
Treatment history demonstrates that worsening conditions aren’t due to lack of treatment engagement. DBQs show active treatment participation while symptoms worsened despite these efforts.
Medication trial documentation includes specific medications tried, dosages, duration of treatment, side effects experienced, and effectiveness levels. This comprehensive medication history shows treatment resistance that supports higher ratings.
Therapy participation records demonstrate consistent engagement with evidence-based treatments like Cognitive Processing Therapy or EMDR. Symptom persistence or worsening despite this participation indicates severe, treatment-resistant PTSD.
Occupational Impairment Evolution
Detailed analysis of work performance changes, employment sustainability, and career impact progression since last evaluation provides concrete evidence of functional deterioration. The VA’s rating system heavily weights work capacity.
Performance evaluation changes offer objective evidence of decline. Increasingly negative work reviews, disciplinary actions related to PTSD symptoms, or performance improvement plans document employment deterioration.
Career trajectory analysis shows long-term impact. Stalled promotion tracks, forced career changes, or acceptance of lower-responsibility positions due to worsening symptoms justify higher disability ratings.
Evidence Strengthening Strategies for Increases
Successful increase claims require robust supporting evidence beyond the DBQ itself. Supporting documentation from multiple sources creates a comprehensive picture of condition deterioration.
Increase claim success depends on evidence beyond the DBQ. Multiple documentation sources create a comprehensive picture that the VA reviews during evaluation.
Corroborating Medical Records Integration
Integration of ongoing treatment documentation, hospitalization records, and specialist consultations supports DBQ findings with longitudinal evidence. This shows consistent symptom reporting and treatment engagement across multiple healthcare providers.
Medical records from ongoing treatment provide crucial corroboration. These records should show consistent symptom reporting that aligns with DBQ findings and demonstrates progression over time.
Emergency room visits for panic attacks, psychiatric hospitalizations, or crisis interventions provide evidence of symptom severity. These acute care episodes demonstrate condition severity requiring immediate intervention.
Specialist consultations with psychiatrists, psychologists, or trauma specialists add credibility to increase claims. When multiple independent medical professionals document similar findings, it strengthens the overall medical record.
Lay Statement Integration
Family, friend, and colleague observations provide functional impairment evidence that complements clinical findings. These statements offer real-world examples of symptom impact that medical professionals might not observe during brief evaluations.
Lay statements from people who interact with veterans regularly provide evidence that clinical evaluations might miss. These statements focus on specific behavioral changes observed since the last rating decision.
Spousal statements carry particular weight because spouses observe daily functioning that others don’t see. They can document sleep disturbances, mood changes, social withdrawal, and relationship difficulties affecting quality of life.
Workplace colleague statements can document occupational impairment progression. Coworker observations of increased irritability, concentration problems, or social withdrawal support DBQ findings with real-world functional evidence.
Recent Senate hearings have reinforced the legitimacy of PTSD claims, with Sen. Richard Blumenthal stating that fraud investigations target only 3.7% of cases, with most focusing on external scammers rather than veterans, according to Disabled Veterans. This congressional support validates the importance of thorough increase claim documentation.

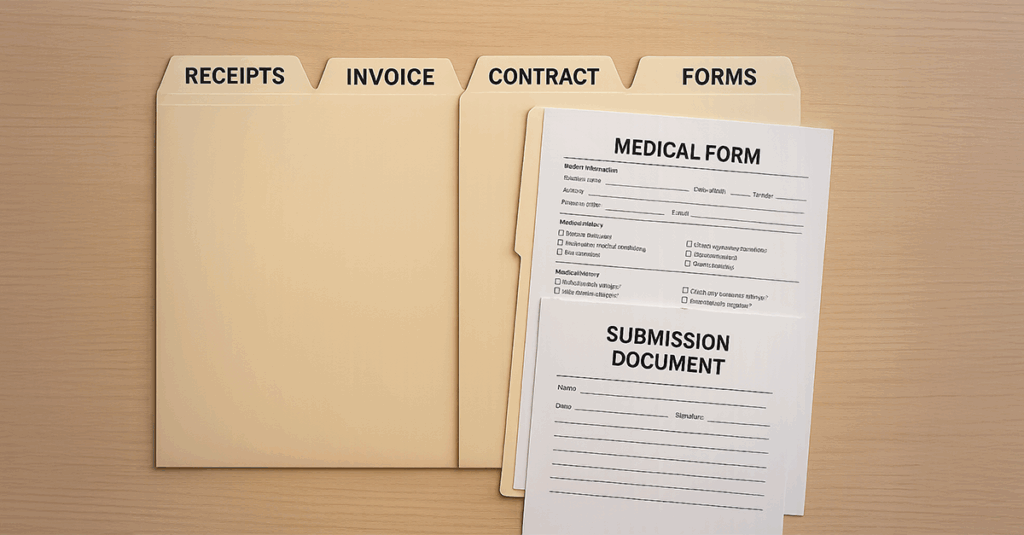
VA DBQ Form Standards
Proper DBQ form handling requires attention to specific VA formatting, terminology, and documentation standards that differ from standard medical practice. This includes precise medical opinion language and functional limitation specificity.
The VA processes DBQs according to specific requirements. Understanding these procedural standards prevents delays and rejections that could set cases back months or years.
Form Completion Best Practices
Accurate DBQ completion requires mastery of VA-specific formatting, terminology, and documentation standards that align with processing requirements. This includes precise medical opinion language using specific probability terms and detailed functional limitation descriptions.
DBQ completion strategy needs to account for how VA raters process these forms. Raters look for specific information presented in standardized formats, requiring documentation that speaks their language.
Medical Opinion Clarity
DBQ medical opinions must use precise probability language like “more likely than not” or “at least as likely as not” for service connection determinations. This avoids ambiguous clinical language that creates processing delays or denials.
Medical opinion language significantly affects claim outcomes. The VA operates on probability standards rather than clinical certainty. Medical professionals need to understand that “possible” or “could be related” doesn’t meet VA standards for service connection.
The specific terms “more likely than not” (greater than 50% probability) and “at least as likely as not” (50% or greater probability) align with VA service connection standards. Medical opinions should also address alternative causation when relevant.
Functional Limitation Specificity Requirements
Detailed descriptions of specific functional limitations must replace vague terminology. This provides clear rating criteria alignment through concrete examples of occupational and social impairment that VA decision-makers can translate into disability percentages.
Functional limitation documentation requires concrete examples rather than clinical generalizations. Effective DBQs describe specific impacts like inability to maintain friendships, work environment limitations, or sleep disturbance effects rather than general impairment statements.
Work-related limitations need specific examples addressing open office environments, break frequency needs, customer service capacity, and interpersonal interaction abilities. Sleep disturbance documentation should include specific impacts on work performance and family interactions.
Psychosocial DBQ Integration for PTSD
In VA-conducted initial PTSD evaluations, psychological DBQs incorporate comprehensive psychosocial assessments evaluating PTSD’s impact across multiple life domains. This includes social functioning, family relationships, and educational/vocational capacity evaluation.
PTSD affects multiple life aspects, and comprehensive DBQ documentation captures this broad impact through detailed psychosocial assessment beyond symptom checklists.
Social Functioning Assessment Strategies
Documentation of interpersonal relationship difficulties, social isolation patterns, and community engagement limitations provides functional impairment evidence that supports disability rating determinations.
Social functioning assessment requires specific examples of relationship difficulties. The VA considers how PTSD affects marriages, friendships, and social gathering participation that was previously enjoyed.
Community engagement documentation shows broader social impact. Discontinued participation in religious activities, volunteer work, or recreational clubs demonstrates significant functional impairment.
Interpersonal relationship patterns need detailed analysis. Difficulty trusting others, social isolation, or inappropriate anger in social situations directly correlate with VA rating criteria.

Family Impact Documentation
Assessment of PTSD’s effects on spousal relationships, parenting capacity, and family dynamics supports disability rating determinations. The VA reviews how symptoms disrupt family functioning and create additional stressors.
Family impact documentation demonstrates real-world functional impairment. The VA considers how PTSD affects spousal and parental roles and whether family relationships deteriorated due to symptoms.
Parenting capacity assessment addresses specific limitations including patience during parenting tasks, emotional connection with children, and anger management issues affecting parenting effectiveness.
Spousal relationship documentation might include decreased intimacy, communication difficulties, or increased conflict due to PTSD symptoms. These relationship impacts demonstrate significant functional impairment.
Educational and Vocational Capacity Evaluation
Evaluation of concentration difficulties, memory problems, and learning impairments that affect educational pursuits and job training capabilities provides additional functional limitation evidence.
Educational capacity assessment addresses ability to pursue further education or job training. The VA reviews whether concentration difficulties prevent coursework completion or memory problems affect skill acquisition.
Vocational capacity evaluation considers career limitations beyond current employment. The VA reviews what work environments trigger symptoms and what job responsibilities cannot be handled due to PTSD.
Learning impairment documentation might include difficulty processing new information, retention problems, or focus inability during training sessions. These cognitive impacts demonstrate additional functional limitations.

VA-Specific DBQ Requirements and Standards
VA DBQ completion must adhere to specific agency requirements following 38 CFR guidelines and VA Manual M21-1 standards. This requires specialized knowledge of rating criteria and internal processing protocols.
The VA operates under specific regulatory requirements that differ from standard medical practice. DBQs need to meet these agency-specific standards to avoid processing delays or rejections.
Regulatory Compliance Standards
DBQ completion must follow 38 CFR guidelines and VA Manual M21-1 requirements to ensure acceptance and proper processing by regional offices. This requires familiarity with specific formatting, terminology, and documentation standards unique to VA disability claims.
Regulatory compliance affects claim processing. The VA’s processing system expects specific information presented in standardized formats. Deviation from these standards creates processing delays and potential denials.
38 CFR Part 4 provides the rating schedule framework that DBQs must address. Understanding how symptoms align with specific rating criteria helps ensure DBQs provide the necessary information for accurate rating decisions.
VA Manual M21-1 contains procedural requirements that affect how DBQs are processed. Familiarity with these procedures helps ensure documentation meets processing standards and avoids common pitfalls that delay claims.
Quality Assurance Considerations
Review processes verify DBQ completeness, accuracy, and alignment with VA standards before submission. This prevents delays or rejections by ensuring all required elements are properly documented and formatted according to agency specifications.
Quality assurance review verifies that DBQs address all required elements before submission. Missing information or improper formatting creates development requests that delay claim processing by months.
Documentation accuracy review ensures that all statements are supported by evidence and that medical opinions meet VA probability standards. Inconsistencies between different DBQ sections can trigger additional development or denials.
VA standards alignment verification confirms that DBQs use appropriate terminology and address specific rating criteria. This final review prevents common errors that undermine otherwise strong claims.
| DBQ Component | VA Requirement | Processing Impact |
| Medical Opinion | Must use “more likely than not” or “at least as likely as not” language | Inadequate probability language triggers development requests |
| Functional Limitations | Requires specific examples with frequency/severity metrics | Vague statements prevent accurate rating assignment |
| Service Connection | Needs chronological timeline from trauma to current symptoms | Timeline gaps create service connection doubts |
| Symptom Documentation | Must align with DSM-5 criteria and VA rating schedules | Non-aligned documentation delays processing |
Complex PTSD Evaluation Considerations
Complex PTSD cases require specialized DBQ approaches addressing comorbid conditions, treatment-resistant symptoms, and unique presentation patterns that standard evaluations may miss. This demands nuanced documentation strategies that separate overlapping conditions while acknowledging their interconnected nature.
Not all PTSD cases fit standard evaluation templates. Complex presentations involving multiple mental health conditions, treatment resistance, or unique symptom patterns require sophisticated DBQ approaches.
Comorbidity Documentation Strategies
PTSD frequently co-occurs with other mental health conditions, requiring careful DBQ documentation that separates and integrates multiple diagnostic considerations. This addresses depression and anxiety integration, substance use disorder considerations, and their combined functional impact.
Comorbid mental health conditions create documentation challenges because symptoms often overlap, making it difficult to determine which condition causes specific functional limitations. DBQs need to address this complexity while maintaining clarity for rating purposes.
Depression and Anxiety Integration
Clear documentation distinguishes PTSD-specific symptoms from overlapping depression and anxiety manifestations while acknowledging their interconnected nature. This provides separate functional impact assessments that support appropriate ratings for each condition.
Depression and anxiety symptoms frequently overlap with PTSD, creating diagnostic complexity that affects rating decisions. DBQs need to separate these conditions while acknowledging their interconnected nature and combined impact on functioning.
PTSD-specific depression often relates directly to trauma themes including guilt about survival, shame about trauma response, or hopelessness about recovery. This trauma-related depression differs from major depressive disorder and requires separate documentation.
Anxiety symptoms in PTSD typically involve hypervigilance, exaggerated startle response, and trauma-related fears. These differ from generalized anxiety disorder symptoms and need distinct documentation that supports separate ratings when appropriate.
Substance Use Disorder Considerations
Assessment of substance use as PTSD self-medication versus independent addiction requires nuanced clinical judgment and specialized documentation approaches. This addresses causation, treatment implications, and combined functional impact on disability ratings.
Substance use disorders frequently co-occur with PTSD, but the relationship between these conditions affects rating decisions. The VA considers whether substance use represents self-medication for PTSD symptoms or an independent condition that complicates treatment.
Self-medication patterns need specific documentation including what substances are used, when they’re used in relation to PTSD symptoms, and how they affect symptom management. This pattern suggests PTSD as the primary condition.
Independent substance use disorders require separate documentation of addiction patterns, treatment history, and functional impact. When both conditions exist independently, they may warrant separate disability ratings reflecting their combined impact.
Research shows that veterans of Operations Iraqi Freedom and Enduring Freedom have PTSD rates of 29% at some point in their lives, according to Hill & Ponton, with many of these cases involving complex comorbidities requiring specialized documentation approaches.
Treatment-Resistant PTSD Documentation
Veterans with PTSD that doesn’t respond to standard treatments require specialized DBQ approaches capturing symptom severity and persistence despite intervention attempts. This includes comprehensive medication trial documentation, therapy outcome analysis, and alternative treatment considerations.
Treatment-resistant PTSD presents unique documentation challenges because symptom persistence despite appropriate treatment suggests severe, chronic conditions. DBQs need to capture this treatment resistance comprehensively.
Medication Trial Documentation
Comprehensive record of failed medication trials, adverse reactions, and partial response patterns supports disability rating determinations for treatment-resistant cases. This demonstrates that symptom persistence occurs despite appropriate pharmacological intervention attempts.
Medication trial documentation requires detailed records of specific medications tried, dosages reached, duration of treatment, side effects experienced, and effectiveness levels achieved. This comprehensive history demonstrates treatment resistance.
Failed medication trials should include reasons for discontinuation including lack of effectiveness, intolerable side effects, or medical contraindications. Each failed trial strengthens the case for treatment-resistant PTSD.
Partial response documentation shows that while some improvement occurred, significant symptoms and functional limitations persist despite optimal medication management. This partial response pattern supports ratings that reflect ongoing impairment despite treatment.
Therapy Outcome Analysis
Documentation of limited improvement despite evidence-based therapy participation in treatments like CPT, EMDR, and PE demonstrates symptom severity and chronicity. This supports disability rating determinations for treatment-resistant presentations.
Therapy outcome analysis requires documentation of specific evidence-based treatments attempted, duration of participation, compliance with treatment recommendations, and outcomes achieved. Limited improvement despite appropriate therapy suggests severe, treatment-resistant PTSD.
Cognitive Processing Therapy (CPT) outcomes should document specific modules completed, homework compliance, and symptom changes throughout treatment. Limited improvement despite full CPT participation indicates treatment resistance.
EMDR therapy documentation needs to address specific trauma memories processed, number of sessions completed, and degree of trauma resolution achieved. Persistent trauma symptoms despite adequate EMDR treatment supports disability rating determinations.
Alternative Treatment Considerations
Assessment of non-traditional treatment attempts, including their outcomes and limitations, provides comprehensive clinical picture for rating purposes. This demonstrates exhaustive treatment efforts and persistent symptom severity despite diverse intervention approaches.
Alternative treatment documentation shows comprehensive treatment efforts that extend beyond standard interventions. This may include acupuncture, meditation, yoga therapy, or other complementary approaches. Limited success with these treatments further demonstrates symptom severity.
Residential treatment program participation provides evidence of severe symptoms requiring intensive intervention. Documentation should include program duration, treatment components, discharge status, and post-treatment functioning levels.
Experimental treatment participation, such as ketamine therapy or clinical trials, demonstrates pursuit of available treatment options. Limited success with these cutting-edge approaches further supports treatment-resistant PTSD considerations.
Treatment-Resistant PTSD Example: A Marine veteran with combat PTSD completed 12 weeks of CPT, 20 sessions of EMDR, tried 8 different medications over 3 years, participated in a 30-day residential program, and attempted alternative treatments including acupuncture and meditation. Despite this comprehensive treatment history, daily panic attacks, chronic insomnia, and inability to maintain employment continued. In this scenario, the DBQ documented this treatment-resistance pattern, and the VA ultimately assigned a 70% rating increase from the previous 50% rating based on its review of the overall evidence.
Recent developments in VA oversight highlight the importance of thorough DBQ documentation, with VA Inspector General Cheryl Mason noting that public-facing DBQs pose ‘significant risk’ due to incomplete or questionable submissions, according to Disabled Veterans, emphasizing the need for comprehensive, accurate documentation in complex cases.
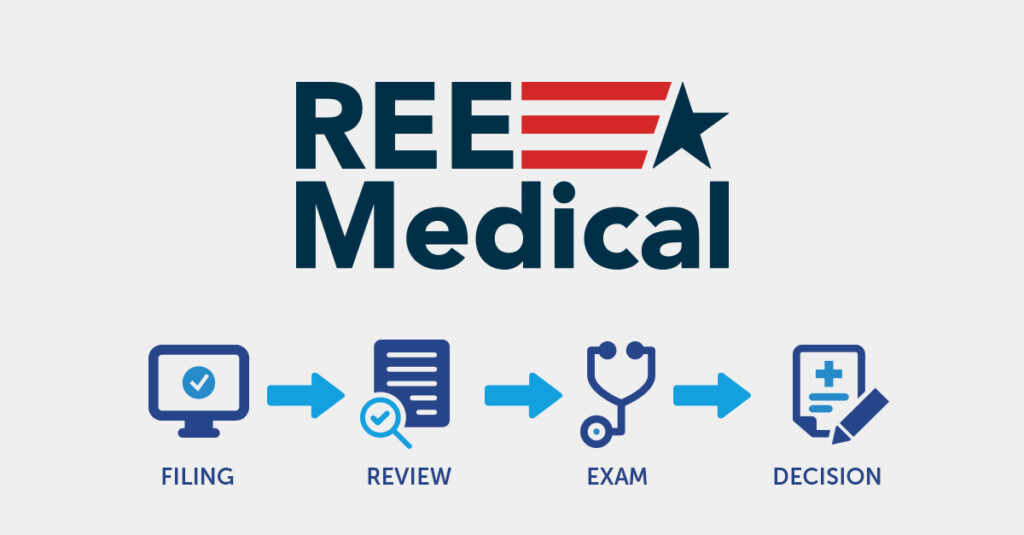
How REE Medical Coordinates Comprehensive PTSD Evaluations
REE Medical coordinates access to a nationwide network of independent, licensed medical professionals who are familiar with trauma-informed assessment approaches. These independent providers conduct clinical evaluations and document findings related to PTSD and any comorbid conditions, treatment history, and symptom patterns. These independent evaluations do not replace the VA’s own Initial PTSD DBQ for first-time PTSD claims; instead, they may serve as additional medical documentation that the VA can review, particularly in connection with review or rating increase claims.
Whether a veteran is dealing with complex comorbidities, treatment-resistant symptoms, or concerns about condition changes, REE Medical connects them with independent medical professionals who focus on detailed clinical PTSD documentation. REE Medical’s flat-rate pricing model is designed to provide transparency around evaluation costs and does not involve contingency fees or a percentage of VA benefits.
Veterans can contact REE Medical for an informational consultation to learn how independent medical evaluations are coordinated and how this clinical documentation may be used as medical evidence that the VA can review in connection with a disability claim. These consultations are educational in nature and are not a substitute for medical care, legal advice, or assistance from an accredited representative.
Final Thoughts
The PTSD DBQ serves as foundational medical evidence that the VA reviews during disability evaluations. Understanding how these forms function within the VA system helps veterans recognize what medical documentation the VA considers when making rating decisions.
The difference between rating percentages can represent significant financial impact over a lifetime. Comprehensive DBQ documentation helps capture condition complexity and functional impact, providing the VA with medical information it may consider when evaluating disability claims.
Whether pursuing initial claims, seeking increases, or addressing complex comorbidities, the clarity and completeness of DBQ documentation can affect how the VA evaluates the evidence in a claim. Veterans may wish to work with qualified medical professionals who can document the full impact of service-connected conditions within the VA’s evidentiary framework.
PTSD DBQ Documentation Considerations
Veterans preparing for disability evaluations may benefit from gathering comprehensive medical records from service and post-service treatment, documenting specific traumatic events with dates and locations, collecting lay statements from family and colleagues, preparing detailed symptom timelines, listing all medications tried with effectiveness information, documenting all therapy attempts and outcomes, gathering employment records showing performance changes, preparing specific examples of functional limitations, ensuring medical examiners understand VA probability language requirements, and reviewing DBQ forms for completeness.
The PTSD DBQ represents more than paperwork in the VA’s evaluation process. The VA needs to see how PTSD affects daily life, relationships, work capacity, and overall quality of life. This comprehensive medical picture, when properly documented through clinical evaluation, provides the VA with additional information it may review as part of its disability assessment. The VA alone determines how much weight to give any particular evidence and what disability rating to assign.
DISCLAIMER
DISCLAIMER: REE Medical, LLC is not a Veterans Service Organization (VSO) or a law firm and is not affiliated with the U.S. Veterans Administration (“VA”). Results are not guaranteed, and REE Medical, LLC makes no promises. REE Medical’s staff does not provide medical advice or legal advice, and REE Medical is not a law firm. Any information discussed, such as, but not limited to, the likely chance of an increase or service connection, estimated benefit amounts, and potential new ratings, is solely based on past client generalizations and not specific to any one patient. The doctor has the right to reject and/or refuse to complete a Veteran’s Disability Benefit Questionnaire if they feel the Veteran is not being truthful. The Veteran’s Administration is the only agency that can make a determination regarding whether or not a Veteran will receive an increase in their service-connected disabilities or make a decision on whether or not a disability will be considered service-connected. This business is not sponsored by, or affiliated with, the United States Department of Veterans Affairs, any State Department of Military and Veterans Affairs, or any other federally chartered veterans service organization.